Oct 09, 2019
Enhancing Services for Deaf, Hard of Hearing, and Deafblind Patients in Rural America
by Allee Mead
Trish Leakey, JD, is a Deaf individual with Deaf parents. Before the Americans with Disabilities Act was passed in 1990, her family had to rely on written notes, gestures, and family members to talk with employers, schools, and healthcare providers. However, the other family members did not know American Sign Language (ASL), so they gave what Leakey called “bumper-sticker summary” translations and took over decision-making at meetings and appointments.
The world opened up to my family after the ADA was passed. We had access to qualified, professional sign language interpreters who were well-trained; knew our language; had the correct vocabulary for various settings, like medical vocabulary; and abided by a Code of Professional Conduct, which meant they respected principles of confidentiality and maintained proper boundaries.
“The world opened up to my family after the ADA was passed,” Leakey said. “We had access to qualified, professional sign language interpreters who were well-trained; knew our language; had the correct vocabulary for various settings, like medical vocabulary; and abided by a Code of Professional Conduct, which meant they respected principles of confidentiality and maintained proper boundaries.”
Now, while traveling through Colorado as the Auxiliary Services Manager at the Colorado Commission for the Deaf, Hard of Hearing, and DeafBlind (CCDHHDB), Leakey said she has “seen things that remind me of my youth”: a lack of qualified sign language interpreters in rural communities. Even when rural patients can get an interpreter, it's expensive for the interpreter to travel from the urban Front Range.
Timothy Chevalier, Ed.D., CCDHHDB Outreach Consultant, shared a similar experience in his work. This lack of services, he said, “equates to a lack of access and results in unequal access to vital programs, services, and events in fields such as legal, medical, and educational.” CCDHHDB is working to remove some of those barriers to access.
Definitions of Deafness and American Sign
Language
According to Information Gaps on the Deaf and Hard of
Hearing Population: A Background Paper (2006) (no
longer available online), the term
“deaf” refers to the physical
condition in which someone's degree of hearing acuity
is such that the person would not benefit from a
hearing aid. The term “Deaf” refers
to those who self-identify with Deaf culture, in which
being deaf is not a disability but part of one's
identity, like ethnicity or religion. Deafblind people,
according to the Helen Keller Center website (2019),
“have some degree of combined vision and
hearing loss.”
American Sign Language (ASL) is the predominant language used by Deaf people in the United States. It is a visual language with a unique grammar and syntax, which differs from English.
Barriers to Health
There are two types of barriers to healthcare for those who are Deaf and hard of hearing (DHH): lack of accommodations and inadequate clinician training. Lack of accommodations includes not having a sign language interpreter present at the healthcare setting or not having devices like hearing aids available for patients. In addition, many clinicians don't receive training about Deaf culture, the values of visual access for communication, or how to effectively communicate with DHH patients.
“These issues can be exacerbated in rural areas,” University of Michigan associate professor Michael McKee, MD, MPH, said, especially “with low availability of sign language interpreters.” In addition, rural healthcare facilities may not have critical care managers, care navigators, or social workers to individually work with patients and help them get the care and accommodations they need.
Communication barriers between patients and providers can lead to serious health problems. McKee, who directs the Deaf Health Clinic in Dexter, Michigan, shared stories of DHH patients who were diagnosed by previous providers with diabetes and chronic pain but never received lifestyle coaching. Some patients with poorly controlled diabetes were still taking oral diabetes medications even though they were truly insulin-dependent. Some patients with chronic pain were just prescribed narcotics, which led to opioid dependency and addiction.
“We have several patients who were not treated with anticoagulants even though they had atrial fibrillation and were at high risk for stroke,” said McKee, who has a hearing loss. “This was due to their inability to communicate on the risks of bleeding from these medications.”
McKee said, “Healthcare providers generally are poor judges on whether their health communication is effective or not. Part of this is the lack of training opportunities on how to effectively communicate with many of our patients and other staff members. This is despite the fact that most healthcare errors are due to communication failures.”
I would recommend that providers ask their DHH patients about how they can achieve effective communication. They also need to understand that they are responsible for any accommodations, such as cost, to ensure this.
He added, “I would recommend that providers ask their DHH patients about how they can achieve effective communication. They also need to understand that they are responsible for any accommodations, such as cost, to ensure this.”
Healthcare providers can improve communication by honoring how the Deaf culture values visual access, such as facing the patient, making good eye contact, and making sure your face is not obscured, so that patients who read lips are able to see the provider when he or she is speaking. DHH patients, along with patients with other communication-based needs or whose first language isn't English, may also benefit from longer office visits.
In addition, don't speak too fast or use jargon, McKee said. Use visual aids when applicable and teach-back strategies so you can verify whether or not a patient understands what you've said or double-check the accuracy of the interpretation. Of course, strategies like plain language and asking questions can benefit all patients.
Effective Ways to Communicate with Deaf and
Hard of Hearing Individuals
These tips are adapted from the CCDHHDB resource
Communication Tips For Individuals Who Are Hard of Hearing and the
Eight Step Advocacy Plan for Deaf and Hard of Hearing
Survivors of Sexual Assault: A Guide for Rural
Dual/Multi-Service Advocates:
- Use plain language, not jargon. Someone may hear you but not understand what you're saying. In addition, plain language is easier to lip-read.
- Ask patients what their preferred method of communication is. If a patient prefers to lip-read, speak at your normal speed and don't cover your mouth.
- Look at the patient (not the interpreter) when the patient is speaking, and make sure you don't speak unless the patient is looking at you. For example, don't talk while they're filling out forms.
- If there are more than two people in the conversation, make sure you take turns speaking to avoid overlapping conversations.
- Make sure the facility is well-lit so that patients can see your face and hands. In addition, don't sit in front of bright lighting (for example, in front of a window).
- Be aware of other environmental distractions, like too many posters on the wall.
- Hearing aids amplify all sounds equally, so someone might still struggle to hear you if there is background noise.
The Deaf Health Clinic also uses door knock light alarms (a light flashes when someone knocks) to let patients know when a healthcare staff member wants to enter the room. The clinic, which has ASL staff members on the team, also asks its patients for their communication preferences and lists those in individual patients' records.
The clinic also offers telemental health. “Telehealth can allow for rural individuals to access care at a specialized clinic like ours,” McKee said. “We provide both mental health counseling and medication reviews through these visits.”
However, technology isn't necessarily a cure-all. Video Remote Interpreting (VRI) is similar to telehealth but with an interpreter operating remotely instead of a healthcare provider. VRI can be effective in some situations but inappropriate in others, said Elizabeth Hill, Director of the New Jersey Division of the Deaf and Hard of Hearing (DDHH).
For example, if it's a short appointment or if the healthcare staff is using VRI until an interpreter arrives in person, VRI can work. In rural areas, VRI may be the only option if there are few or no local interpreters available. The technology has limitations. In some cases, VRI screens may be too small, making it difficult for the patient to see the interpreter. In addition, the video speed can be too slow — in which case the interpreter's signs will be choppy or frozen — or the equipment itself is tethered and can't be moved to better accommodate patients who are immobilized. Even if a healthcare facility has VRI or has a policy to only use VRI, the patient still has the right to request an in-person interpreter.
Many of our DHH patients, through numerous negative experiences or healthcare visits without good communication, are disempowered. We try to help them feel empowered again. I inform them of their patient rights and also ask them to be a partner to their health.
“Many of our DHH patients, through numerous negative experiences or healthcare visits without good communication, are disempowered,” McKee said. “We try to help them feel empowered again. I inform them of their patient rights and also ask them to be a partner to their health.”
McKee also warned against relying on DHH patients' hearing family members. Professional interpreters are trained to be impartial and confidential, whereas family members are emotionally involved in the patient. “Family members can be very helpful,” McKee said, “but their involvement may vary depending on the needs of the DHH patient. It is important to engage the DHH patient directly rather than trying to go through family members. Family members should not be used as interpreters.”
Even staff members who know some ASL are not enough, said Hill: “Interpreters are professionals with specific training and certification.” She encouraged people to learn ASL but emphasized that conversational ASL is different from the work of a professional interpreter.
Providing Deaf Sensitivity Training
The New Jersey DDHH frequently receives calls from healthcare providers asking for information and referral when they are presented with a patient who is deaf or hard of hearing. Healthcare providers may not fully know or understand their obligations as a public accommodation to provide effective communication under the ADA. In addition to consultation with healthcare providers, case management services, a hearing aid project, and an equipment distribution program, the New Jersey DDHH provides deaf sensitivity training to any organization, state agency, or community service that requests it.
This training gives an overview of Deaf culture and effective communication strategies. Participants learn that American Sign Language (ASL) is a distinct language and may be many deaf people's native language.
For providers, the training has shed light on common but ill-informed practices. “In many cases, healthcare providers chose to use written notes in lieu of providing qualified ASL interpreters to communicate complex information,” Hill said, “but that leads to situations where the deaf person did not have an understanding of what was being communicated,” since English may be that patient's second language. In addition, providers might not think to use plain language when writing something down, like saying myocardial infarction instead of heart attack, which can confuse patients.
The trainings also reveal common misconceptions about DHH people. For example, Hill remembers a participant who, during a true/false quiz, confidently said that deaf people couldn't drive. When the training instructor told her that they could, she asked how they could hear the horn. “When your music is blasting, how do you hear the horn?” the instructor asked. The participant realized that hearing wasn't essential to driving. “Clearly, education about deaf people's abilities is still very much needed,” Hill said.
The New Jersey DDHH's deaf sensitivity training covers:
- Common challenges, impact, and range of hearing loss
- Strategies for effective communication
- How and when to request communication access
services such as:
- Sign language interpreters, including deaf interpreters
- Specialized interpreters, such as a tactile interpreter for someone who is deafblind
- Communication Access Realtime Translation (CART), which prints out what is being said, for those who prefer to read text
- Communication access laws
- Information on New Jersey DDHH services
Hill's office also offers resources that providers can
recommend to their patients who may have deaf or hard of
hearing children. ASL Deaf Language Associates are deaf
adults fluent in ASL who can help with language
acquisition and development. They can work with children
in childcare settings, preschool programs, or at
someone's home for up to 25 hours a week. This program is
open to deaf, hard of hearing, and deafblind children
ages 0-5. Children who will communicate primarily by
speaking can still benefit from sign language support in
their language development.
Healthcare providers are a critical part of getting information out there and connecting families with the services they need.
Hill said, “Healthcare providers are a critical part of getting information out there and connecting families with the services they need.”
Bringing Interpreters to Rural Settings
The CCDHHDB Auxiliary Services program in Colorado provides individuals with access to qualified sign language interpreting services, CART services, and auxiliary aids. It serves the Colorado State Courts and administrative courts, rural areas of Colorado, and selected State Executive branch agencies.
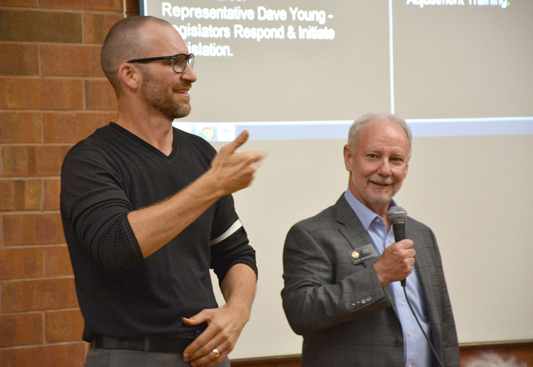
In July 2018, the CCDHHDB received a two-year grant from the Colorado General Assembly's Joint Budget Committee for the Rural Interpreting Services Project (RISP). RISP (now Rural Auxiliary Services) works to bring sign language interpreting services to rural areas, train interpreters at the initial and advanced level, and conduct community outreach. RISP interpreting services — available for medical, legal, employment, or other situations — are free for the consumers as well as the providers.
RISP came from a meeting between the Joint Budget Committee and rural advocacy groups to discuss the communication barriers that individuals who are deaf, hard of hearing, and deafblind face in rural communities. These barriers include the lack of onsite sign language interpreters and the travel costs of driving in interpreters from urban areas.
In addition, a mentoring program partners more experienced interpreters with beginners. Mentoring prepares beginners for situations that might not have been covered in a sign language interpreting program. “Sign language interpreting is a complicated field, requiring mastery of a language and culture as well as an ability to process and facilitate communication,” Leakey said.
My observation is that mentoring promotes language/interpreter proficiency because it provides the protégée with an opportunity to be guided with constructive feedback by a veteran interpreter while working with a deaf individual who is the language model.
Chevalier, who was raised by Deaf parents in South Dakota, said, “My observation is that mentoring promotes language/interpreter proficiency because it provides the protégée with an opportunity to be guided with constructive feedback by a veteran interpreter while working with a deaf individual who is the language model.” He added that the program builds protégées' self-confidence and builds bridges between interpreters and the deaf community.
The CCDHHDB recruited interpreters for RISP by reaching out to all the community-based interpreters (as opposed to educational interpreters who work in classrooms) in Colorado listed in the Registry of Interpreters for the Deaf (RID). Colorado law requires those calling themselves “sign language interpreters” to be certified by RID. RISP currently has 29 agencies and freelance interpreters participating in the project.
RISP also partnered with the University of Northern Colorado's Department of American Sign Language and Interpreting Studies to offer RISP scholarships for undergraduate students and a Certification Readiness Training (CRT) program for signers who currently live in rural Colorado or are willing to work there. So far, 21 participants from 16 counties have been accepted to CRT and will complete a one-year online training program.
RISP provides outreach to let rural communities know how they can receive free interpreting services. So far, RISP staff have held 10 town hall meetings for healthcare providers and deaf, hard of hearing, and deafblind individuals in the communities of Alamosa, Breckenridge, Durango, Frisco, Granby, Grand Junction, La Junta, Fort Morgan, Pueblo, and Steamboat Springs.
As the outreach consultant, Chevalier has put in more than 600 hours in outreach services by contacting communities about RISP. He works with local media, ADA coordinators, human resources staff, and local independent living centers with deaf services.
RISP staff conducted surveys at the RISP town hall meetings, and 70% of attendees/providers said they serve deaf, hard of hearing, and deafblind individuals at least once a month. Between July 2018 and April 2019, RISP has completed 421 interpreting requests from 30 counties. The majority of requests came from four rural counties: Mesa (133 requests), Alamosa (72), Pueblo (37), and Grand (32). Of the 421 interpreting requests, 279 were medical-related, including mental health and dental services.
The project is making a difference for patients as well as healthcare staff. Leakey shared this testimonial from a provider in southwest Colorado: “At our clinic this morning, we had the opportunity to use RISP for the first time. It was an incredible experience for our patients and for our staff to have a real person interpret as opposed to our video ASL services! It was a great success and the information has now been shared with all of our locations. What an incredible resource!”
Additional Resources
- Questions and Answers for Health Care Providers (National Association of the Deaf) – discusses the ADA and different types of interpreters and auxiliary aids.
- National Institute on Deafness and Other Communication Disorders – offers health information on topics like balance as well as training and funding opportunities for researchers.

