Futures Without Violence in Tillamook County
- Need: To address intimate partner violence (IPV) in primary care settings as a health concern. To increase healthcare providers' professional understanding about its prevalence and adverse impacts on patient health.
- Intervention: In partnership with Safer Futures, Tides of Change provides an advocate at a local health clinic to give confidential services to IPV survivors and training to medical staff. The advocate uses curriculum and other materials designed by Futures Without Violence.
- Results: Healthcare providers at the clinic reported increased understanding of IPV and its impact on health. As a result, IPV advocates received an increase in referrals from healthcare providers. Patients experiencing IPV reported a reduction in chronic, toxic stress and improved overall health after receiving advocacy services.
Description
Intimate partner violence (IPV) negatively impacts health and often results in the development of chronic conditions such as heart disease, high cholesterol, diabetes, chronic pain, substance use disorders, and depressive symptoms. Across the nation, 1 in 4 women and 1 in 7 men experience intimate partner violence. Research shows that healthcare costs of treating women who experience abuse are approximately 42% higher than non-abused women.
 Futures
Without Violence (FUTURES) is a national nonprofit
working to prevent and end gender-based violence that
disproportionately impacts women and children. As part of
their
Improving Health Outcomes Through Violence Prevention
Pilot Project, FUTURES selected 10 domestic violence
programs and community health centers across the U.S. to
receive financial assistance, training, and support.
During a 10-month period, these pairings partnered to
promote the increased safety and improved health outcomes
of those experiencing IPV.
Futures
Without Violence (FUTURES) is a national nonprofit
working to prevent and end gender-based violence that
disproportionately impacts women and children. As part of
their
Improving Health Outcomes Through Violence Prevention
Pilot Project, FUTURES selected 10 domestic violence
programs and community health centers across the U.S. to
receive financial assistance, training, and support.
During a 10-month period, these pairings partnered to
promote the increased safety and improved health outcomes
of those experiencing IPV.
One such partnership is Oregon's Tides of Change (a member of the Oregon Coalition Against Domestic and Sexual Violence that serves current and past survivors of domestic violence, dating violence, sexual assault, stalking and trafficking), and the Rinehart Clinic & Pharmacy (a Federally Qualified Health Center). Tides of Change is a nonprofit IPV assistance center that also provides an advocate stationed at Rinehart Clinic one day a week. The advocate accepts referrals from healthcare providers and consults with providers on warning signs of IPV that arise during patient exams. When the advocate is not present, the clinic's social workers step in to assist providers in addressing the patient's needs.

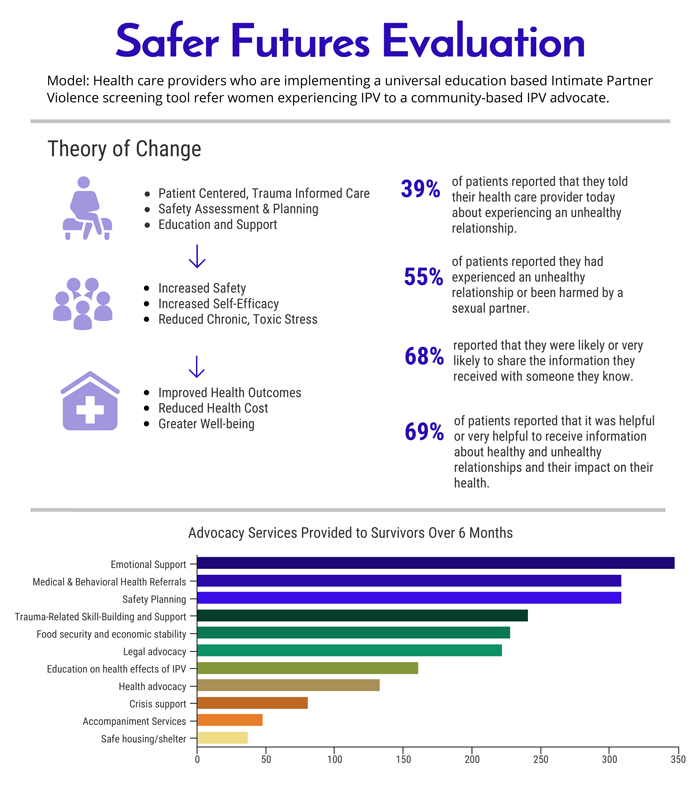
FUTURES screening and intervention tools were first used in Tillamook County as an initiative of the Oregon Department of Justice Safer Futures project – a statewide project that offers IPV advocacy and support in child welfare offices, public health departments, and local primary care clinics. The Safer Futures project operated between August 2013 and July 2017. Support was provided by the Pregnancy Assistance Fund through the Federal Office of Adolescent Health.
This project was funded by several Department of Health and Human Services partners, including the Health Resource and Service Administration (HRSA), the HRSA Office of Women's Health, the Administration for Children & Families, and the Family and Youth Services Bureau.
Funding for Oregon's Safer Futures work comes from the Oregon Department of Justice Victims of Crime Act Assistance Fund and the Ford Family Foundation through October 2019.
Services offered
Through the partnership between Tides of Change and the Rinehart Clinic, the following services are provided to assist multiple audiences:
Healthcare Provider Training
Safer Futures trains healthcare providers on best practices for referrals using FUTURES' National Health Resource Center on Domestic Violence resources and the CUES intervention to address IPV. Brief refresher courses are offered periodically:
- Confidentiality – Disclosing the limits of confidentiality before discussing IPV with patients
- Universal education – The use of safety cards to help patients differentiate between healthy and unhealthy relationships
- Empowerment – Giving each patient two cards, so they can help a friend or family member
- Support – Leaving the patient with referral numbers on the cards and making a warm referral to an advocate when appropriate

Advocates
- The advocate offers free and confidential support services to patients experiencing IPV, including ongoing assessment and safety planning, systems navigation, and connecting them to community and legal resources as appropriate.
- When the advocate is not onsite, the advocacy program staff is available to take referrals over the phone.
Tools, Resources, and Assistance
FUTURES provided the following support to the partnership:
- Quality improvement tools to assess IPV
- Resources to facilitate a productive partnership
- Technical assistance
- Case consultation
- Capacity building support designed to sustain the project beyond grant funding
- Regular leadership team meetings with all 10 participating partnerships
Results
Safer Futures conducted a focus group comprised of Rinehart Clinic's healthcare providers to evaluate the effectiveness of the FUTURES intervention. Providers reported an improved understanding of IPV and its impact on health. They also gained more confidence in talking about IPV with patients and making referrals to IPV advocates.
The clinic now universally screens every patient at the start of the appointment. A change they implemented was "solo patient rooming," allowing for patients to have the privacy to disclose information about their relationship situation.
Because of the risk of disclosure to the partner causing harm, Rinehart Clinic medical staff have taken extra precaution in documenting in a patient's electronic medical record regarding IPV. After a referral is made, documentation occurs in the advocacy group's record keeping system.
Safer Futures also conducted survivor interviews to gauge the impact of healthcare referrals to advocates. The interviews revealed the following results for patients:
- Increased safety
- Increased self-efficacy
- Reduction in chronic, toxic stress
- Improved health
- Reduced fears of reaching out for help
Additional data from the broader Safer Futures cohort of healthcare projects (August 2013 to September 2017):

- Advocates served 955 pregnant women and mothers. Women 20-24 years old represented the largest age demographic served.
- 100% of women agreed that by working with an advocate, they can make informed choices about their situation.
- 97% of women agreed that by working with an advocate, they have new ideas for how to stay safe.
- 100% of women agreed that by working with an advocate, they know more about resources available to them.
- Nearly 500 referrals from healthcare professionals were made to Safer Futures advocates.
- Safer Futures provided 119 trainings to 1,575 Oregon healthcare professionals.
The 2017 Safer Futures Project Evaluation has additional results, including patient and provider feedback from surveys, interviews, and focus groups. In addition, another Oregon information source is the Oregon Guide to Health Care Partnerships.
The partnership between Safer Futures, Tides of Change, and Rinehart Clinic is also featured in the RHIhub Rural Monitor article "Domestic and Intimate Partner Violence: Some Do's and Don'ts for Health Providers."
Having an advocate located at the Rinehart Clinic has given providers and patients direct access to IPV assistance. This has helped providers grow in their confidence to address IPV as a health concern and has continually provided them with a resource to increase their understanding of IPV and how it impacts their patient population.
The on-site advocate also helps break down psychosocial barriers preventing a patient from taking action. Providing assistance in the local setting cuts down on travel time and cost for patients who would otherwise have to travel up to an hour to receive assistance.
Challenges
- Before the start of the project, there was a general lack of understanding about the breadth and depth of IPV in Tillamook County and in the hospital. Many healthcare providers did not understand the role of an IPV advocate as complimentary and distinct from that of licensed clinical social workers. Tides of Change educated healthcare providers about the differences.
- Many patients who experience IPV don't self-identify as survivors or are fearful of potential repercussions of disclosing their situation. Few patients disclose IPV during an exam unless directly asked. Providers have limited time and much to cover during an exam and can easily miss opportunities to identify signs of IPV or related health factors.
- Tides of Change staff initially helped the clinic remove barriers involved with screening in addition to educating medical staff on the risks those who experience IPV encounter when trying to leave. Provider conversation scripts around disclosure and mandatory reporting were also offered.
- Confidentiality is required for any interaction between an advocate and a patient. Advocates do not notify providers if a patient engages in advocacy services or intervention steps. Providers are encouraged to speak directly with their patients about IPV and the services available to them.
- Nonprofit health insurance companies are looking at community solutions to improve healthcare services and reduce cost of IPV for local hospitals and clinics. The Centers for Medicare & Medicaid Services does not reimburse for services provided during appointments with IPV advocates. The most common sources of funding for advocacy and healthcare partnerships in Oregon is grant and foundation funding and charitable contributions.
- Because the clinic advocate is dependent upon non-clinic funding sources, if absent for extended periods of time, referral numbers decline.
- The shift in mindset of medical staff (including providers and medical assistants) toward quality improvement was a challenge. Implementing a screening process required a staff workflow shift, which was guided by a quality improvement process such as Plan-Do-Study-Act (PDSA).

Replication
FUTURES's online toolkit recommends healthcare facilities take the following steps to secure a successful program:
- Build partnerships between healthcare settings and local, community-based IPV organizations.
- Implement an IPV policy that addresses the identification of and response to IPV during exams, promoting prevention, and connecting survivors to IPV programs.
- Educate all patients and staff about the connection between IPV and their health and engage them in strategies to promote wellness and safety.
- Evaluate your progress on a regular basis
FUTURES tools used by Tides of Change and the Rinehart Clinic:
- A Domestic Violence Toolkit for Health Centers & Domestic Violence Programs
- Health Resource Guide: Key Tools
- IPV health tips for healthcare providers and advocates
- Tools for Advocates and the CUES Intervention
- National Conference on Health and Domestic Violence
- Educational videos
- Webinar archives
Tides of Change continues their health partnership work on the local, regional, and state levels to strengthen healthcare response to IPV and identify promising areas for partnership expansions.
Contact Information
Valerie Bundy, Executive Director at Tillamook County Women's Resource CenterTides of Change
503.842.9486
valerie@tidesofchangenw.org
Topics
Abuse and violence
Federally Qualified Health Centers
Women
States served
Oregon
Date added
February 14, 2018
Date updated or reviewed
August 13, 2021
Suggested citation: Rural Health Information Hub, 2021. Futures Without Violence in Tillamook County [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1003 [Accessed 24 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
