Bridges to Care Transitions-Remote Home Monitoring and Chronic Disease Self-Management
- Need: Decrease hospital readmissions and emergency room visits for patients in rural Tidewater, Virginia.
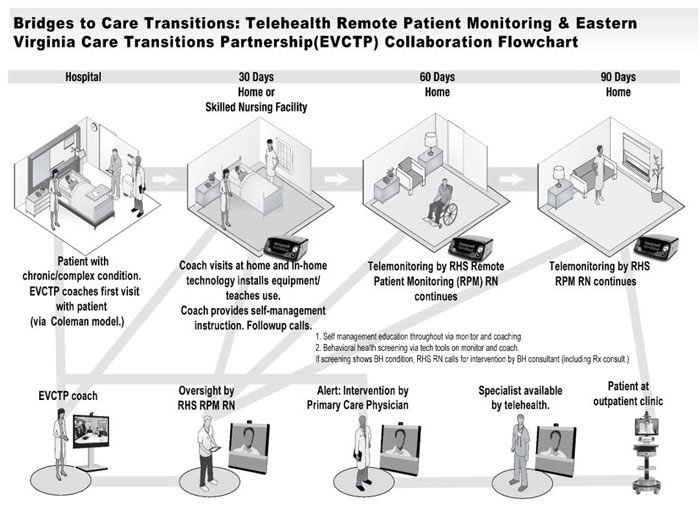
- Intervention: After inpatient admission or ER visit, identify at-risk patients to offer enrollment in remote monitoring and disease self-management education and coaching, with a special focus on behavioral health wellness.
- Results: Decreased readmissions and ER visits paired with high patient satisfaction scores.
Description
Emory University researchers demonstrated that patients with chronic disease and behavioral health issues are high-utilizers of healthcare. According to their personal inpatient discharge research, Riverside Health System found approximately 40% of their patients have a behavioral health condition that may interfere with recovery from an acute illness.
In rural areas, management of these chronic disease and behavioral health conditions is made even more complex by access issues and scarce resources. Nonprofit Bay Rivers Telehealth Alliance (BRTA) collaborates with area organizations in Virginia's Tidewater area to research how remote telehealth monitoring can offset these challenges with its "Bridges to Care Transitions-Remote Home Monitoring and Chronic Disease Self-Management" project.

Two rural hospitals were participants in a remote telemonitoring project. Patients enroll at the time of ER or hospital discharge. Telemonitoring equipment, capable of sharing standard vital signs (blood pressure, oxygenation, weight), is drop-shipped to the patient's home. Soon after, a health coach visits the patient and uses an evidence-based assessment to further assess and build patients' understanding of both their behavioral health and chronic disease challenges.
Specific to this project is a behavioral health wellness assessment. This approach aims to discover eligible patients for the Health Ideas model, a program that provides a health coach for 6 months. If a high-risk patient is identified during screening, they are referred to a behavioral health organization for further care.
Remote monitoring is intended for a recommended 90-day period. Health information is transmitted to the partner health system's coordination center where incoming data are assessed by nurses. Any values outside an expected range are evaluated by phone or home or office visit. Patients not transmitting their data are contacted and patients may also call their health coach or the monitoring center with any questions. Two-week trend data are integrated into the patient's electronic health record allowing primary care providers to review this information in a process similar to the workflow for new lab or X-ray results.
Due to encouraging early results showing improved readmission rates and decreased ER evaluations, BRTA, project partners, and third-party payers are meeting to explore reimbursement models.
This project involves close collaboration with several organizations:
- Riverside Health System
- Middle Peninsula/Northern Neck Community Services Board, a state-funded mental health organization
- Bay Aging
The program is supported by the Federal Office of Rural Health Policy Rural Health Care Services Outreach Project grant. Additionally, BRTA was recognized as a Health Resources and Services Administration (HRSA) 2018 Rural Health Champions for use of evidence-based models in "betterment of rural community health."

Services offered
In-home Equipment
Hardware
- Leased from a for-profit vendor
- Specific for weight, blood pressure, and oxygen saturation monitoring
- Drop-shipped to patient's residence for set-up performed by patient or by patient's family
- If further troubleshooting required, Riverside Health Systems provides phone assistance or onsite tech help (only required for 5% of enrollees)
Software
Software is specific for the selected hardware and uses an internet or wireless connection. If without internet or broadband, a telephonic connection (similar to monitoring heart pacemakers by phone connection) is used.
An additional software feature is a patient query function. Since an electronic tablet for data transmission is used, a condition-related question from the monitoring center can be generated when abnormal results are detected. For example, if a CHF patient has an alert-level weight gain, a question might be sent asking, "Did you need extra pillows to sleep last night?"
Enrollment Care Coordinator Nurses
Participating hospitals' and ERs' care coordinator nurses complete the enrollment process (including consent forms, which is integrated into routine discharge workflow.
Provider Engagement
Project education for discharging providers regarding project objectives and mechanics is required.
Evidence-based Model Integration
The following evidence-based models (EBMs) are used for patient assessment and education:
- The Coleman Model®: Medication management, knowing disease conditions' red flags, healthy behaviors, medical record tracking
- The Healthy IDEAS Model: Behavioral health coaching
- The Stanford Model for Chronic Disease Self-Management
- PHQ-9©
- SBIRT (Screening, Brief Intervention and Referral to Treatment)
- One patient activation-based question
Transition Health Coaches
- Training: Health coaches were hired through Bay Aging's Eastern Virginia Care Transitions Partnership. With backgrounds in varied healthcare fields (for example, community health workers, certified nursing assistants, licensed practical nurses, social workers), these coaches were specifically trained and certified in implementation of the project's evidence-based models.
- Patient Assessment/Education: After installation of home monitoring equipment, coaches make in-home visits for standardized assessment and education. Patients further identified through this process as high risk were referred for more specialized behavioral healthcare.
- Follow-up Visits: Patients/coaches maintain two-way contact by phone or in-home visits as needed.
Remote Patient Monitoring (RPM) Nurses
Remote monitoring software was incorporated into the health system's specialized transfer coordination center. The remote nurse monitoring procedure became part of that center's workflow, a workflow already doing patient-centric activities such as arranging transfers/transport and providing an ask-a-nurse service.
Patients' three main vital signs (oxygen saturation, blood pressure, and weight) come to the center in a "live stream"-like fashion once a day. Time of transmission coordinated with the patient's natural circadian rhythm (for example, 4 a.m. to 1 p.m.) or as needed depending on patient's condition. Alert values were triaged by established algorithms.
Results
Initial project (May 2016-December 2017) enrollee demographics:
- 282 patients: 98 in the study group (grant patients
with RPM and coaching), 184 receiving RPM through home
health (no coaching)
- 41% congestive heart failure (CHF), 28% chronic obstructive pulmonary disease (COPD), 8% pneumonia (PNA), the remaining were other patients identified as high risk for readmission
- 48% Caucasian, 27% African American, remainder unknown
- 52% female, 48% male
- 44% high-risk due to behavioral health conditions
Initial data analysis also demonstrated for grant enrollees:
- 32% had monitoring for ≥ 90 days; less monitoring was often the result of conditions stabilizing or waning patient interest
- Only 10% of enrolled patients needed ER evaluations
- Hospital admissions:
- Overall trend demonstrated that increased length of monitoring time correlated with decreased admissions
- No admissions between 45-day and 90-day monitoring intervals
- 21% of the coached cohort was readmitted and 66% of monitoring-only patients experienced at least one admit during the same time period
Patient satisfaction surveys of patients with remote monitoring plus transitions coaching:
- 75% perceived remote monitoring as improving personal health
- 80% said participation increased self-monitoring motivation
- 95% said participation led to increased self-care for their personal health challenges
- 85% would recommend remote monitoring to others
- Nearly 30% of patients felt remote monitoring was such a valuable service, they wanted it indefinitely and suggested if they had the personal funds, they would pay for the service or at least the coaching without the monitoring.
Challenges
Collateral activity, such as coaching efforts, had funding changes requiring reallocation of grant funds.
Replication
Initial start-up efforts need extensive and thorough planning in order to engage necessary collaborators and vendors, such as hardware/software vendors, coaches, and clinical workflows. (BRTA's previous projects had identified these strategic networks and relationships.)

Equipment decisions should include selected vendor's full disclosure on workflow for repair and malfunction issues. Re-use process should also be identified due to infection concerns associated with equipment colonization with user microbes.
Demonstration equipment is necessary for patient/family education at the time of hospital/ER discharge enrollment since brochures alone were found insufficient for explaining the technology.
In addition to the enrollment process at hospital discharge, consider defining an outpatient enrollment process to accommodate the increased clinician engagement when remote monitoring benefits become evident. (Increased provider engagement has led to another grant opportunity to evaluate outpatients found to be at-risk.)
Family engagement is beneficial, especially with set-up of drop-shipped equipment. However, additional burden for family members must be minimized.
Sustainability was a particular focus of this grant and this discussion needs to be part of initial conversations since current payer reimbursement does not cover expenses. Several current strategies are being entertained. One approach is working at a policy level by sharing data demonstrating reduced hospital and ER visits with area third-party payer sources since results show improved access and decreased costs, especially since patients engaged well with telemonitoring. Though current methods of monitoring are not sustainable by current reimbursement standards, rapid development of new technologic innovations may result in future lower costs.
Contact Information
Donna Dittman Hale, Executive DirectorBay Rivers Telehealth Alliance The Area Health Education Center for the Rappahannock Region
804.443.6286
Execdirector@bayriverstelehealth.org
Topics
Behavioral health
Chronic disease management
Home health
Telehealth
States served
Virginia
Date added
June 14, 2018
Date updated or reviewed
December 23, 2019
Suggested citation: Rural Health Information Hub, 2019. Bridges to Care Transitions-Remote Home Monitoring and Chronic Disease Self-Management [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1016 [Accessed 24 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
