Families Plus Comprehensive Health and Mentoring for Underserved Youth
- Need: Pediatric behavioral health services in Delta County, Colorado.
- Intervention: Multi-organizational and community-wide effort to increase healthcare access for underserved children and to integrate behavioral health care into the area's primary care clinics.
- Results: Sustainable increases in access to pediatric behavioral health services.
Description
 According to the 2018 County Health
Rankings, of Colorado's 58 ranked counties, Delta County
ranked 41st for healthcare outcomes. Local county
needs assessment planning had also revealed that
pediatric behavioral healthcare was a pressing issue.
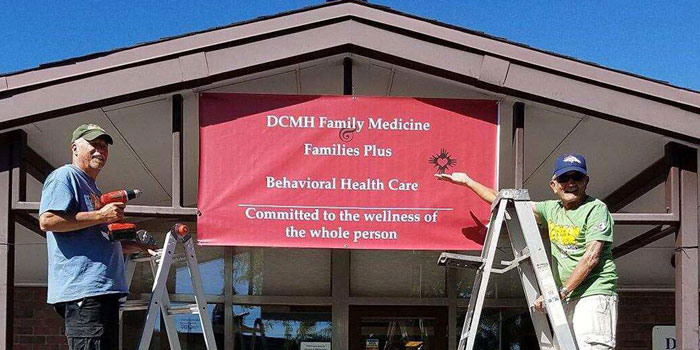
Families
Plus, a nonprofit children's behavioral health
organization in Delta, Colorado, led an effort to
increase behavioral healthcare access to the county's
population age 18 and younger.
According to the 2018 County Health
Rankings, of Colorado's 58 ranked counties, Delta County
ranked 41st for healthcare outcomes. Local county
needs assessment planning had also revealed that
pediatric behavioral healthcare was a pressing issue.
Families
Plus, a nonprofit children's behavioral health
organization in Delta, Colorado, led an effort to
increase behavioral healthcare access to the county's
population age 18 and younger.
Initial strategic community planning created the Delta Consortium and consortium members established 3 main objectives: create access to comprehensive healthcare for underserved children; integrate behavioral health professionals into physical health clinics; and develop community-wide collaboration to promote behavioral healthcare throughout Delta County.
Other county health data was used to identify 3 groups in most need of care: children with complex physical and mental health needs living in family environments with adults with similar needs; children enrolled in clinics with no behavioral healthcare access; and children with an anxiety and depression diagnosis needing mental health therapy in addition to the medication prescribed by the primary care provider.
Using several evidence-based behavioral health models,
the consortium primarily implemented the
Wraparound Model, a model covered by Colorado
Medicaid that uses a process bringing all key agency and
healthcare providers together to build an integrated
treatment plan. The model also focuses on
person-centric/family-centric care drawn from two
components.
 From the
healthcare component, a family/child
unit might select an option for a licensed mental
healthcare professional to follow alongside for an
extended interval. Another choice from this component
might include physical and dental care. From the
community component, choices include
options such as families that mentor, academic tutors, or
enrollment fees for sports programs.
From the
healthcare component, a family/child
unit might select an option for a licensed mental
healthcare professional to follow alongside for an
extended interval. Another choice from this component
might include physical and dental care. From the
community component, choices include
options such as families that mentor, academic tutors, or
enrollment fees for sports programs.
The age of the Families Plus participants were age 3 to 24 and standardized measures tracked progress. Knowing that age 11 is often when children with early trauma begin to struggle, program successes were recognized when youth were able to stay at home and avoid residential care, remain in school, remain free of addiction, and need no legal supervision. Program outcomes demonstrated that 82% of the participating children showed same or improved scores on the Achenbach Child Behavior Checklist and similarly, 92% on the Parent Achenbach Child Behavior Checklist.
Staffing was a key element for the project's launch and Families Plus was able to hire 2 full-time behavioral health professionals. To integrate the behavioral health record into the physical health record, these clinicians developed an electronic health record (EHR) pathway for the three different EHRs used by the primary care clinic consortium members. In addition, these clinicians also developed pathways for use by the primary care providers to more easily navigate the new behavioral health offerings. Due to the clinical language differences between behavioral/physical healthcare, a common vocabulary was created. Billing for behavioral health services — another difference from physical health workflow — was done by a private billing agency.
The original consortium consisted of 4 partners and in three years grew to a total of 9. This growth was also accompanied by a name change to Delta Consortium for Behavioral Health Access. The new consortium is positioned to develop new projects for 2018-2021.
Funding for this project came from the Federal Office of Rural Health Policy's 2015-2018 Rural Health Care Services Outreach Program.
This model was one of 7 Health Resources & Services Administration's 2018 Rural Health Champions and received the Champion in Innovation award.
Services offered
Evidence-based behavioral health models:
- Wraparound Model
- Trauma-focused Cognitive Behavioral Therapy
- Cognitive Behavioral Treatment for Depression
- Universal PHQ-9 depression screening protocols for all consortium members' patients
Results
- 73 individuals participated in the Families Plus model during the third year of the grant.
- 2,045 individuals from the medical clinics participated in depression screening and follow-up during the 3rd year of the grant.
- 88% of mentored children saw their mentor at least four hours a month over a one-year period.
- 93% of Families Plus children had a documented medical visit.
- 85% of Families Plus children had a dental checkup.
- 88% of Families Plus children who were of eligible age enrolled in an activity outside of school. In addition, 39% completed two or more activities.
Other qualitative successes:
- Improved individual health.
- Improved quality of health services.
- Improved capacity for the community to adapt to changes in the local healthcare delivery system.
- Enhanced staff capacity, new skills, and knowledge.
As a result of the project, the local hospital established a behavioral health department and hired two full-time clinicians. Families Plus also continues to work with adult patients in three primary care practices.
After a 2017 planned social media campaign with an estimated 75,000 impressions, sustainability efforts were impacted by increased donations and recruitment of new volunteers to assist with meeting the social determinants of health needs of the area's underserved children.
A "Families Plus Comprehensive Health/Mentoring Model Training Manual" was created.
Challenges
- Time required for the community's guiding leadership to emerge.
- Process of guiding a community's first major healthcare change initiative.
- Modifying 3 separate EHRs.
- Reimbursement for only 80% of total behavioral therapy costs.
Replication
- Initial use of a community-based strategic decision making process can be a positive "game-changer" for engaging a community unfamiliar with a change management process.
- Early identification of effective community leaders from primary care clinics, schools, public health departments, and human services and law enforcement agencies can help provide guidance for the pre-planning and pre-implementation project stages.
- Use stepwise processes for:
- Consortium development.
- Service implementation.
- Understanding the differences between behavioral and physical health care delivery can assist both provider groups to execute a seamless collaboration when services go live.
- Be prepared for additional behavioral health service requests that will arise due to project success within the early adopter physical healthcare provider groups.
- Utilize social media channels.
Contact Information
Brenda Holland, Ph.D., Clinical PsychologistFamilies Plus, Delta, Colorado
970.874.0875
brenda.k.holland@gmail.com
Topics
Access
Child welfare
Children and youth
Families
Integrated service delivery
Mental health
Mental health conditions
Outpatient care
Specialty care
States served
Colorado
Date added
March 22, 2019
Suggested citation: Rural Health Information Hub, 2019. Families Plus Comprehensive Health and Mentoring for Underserved Youth [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1051 [Accessed 19 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
