Sep 11, 2019
Violence Against Hospital Workers: Growing Awareness, Rural Interventions, and Why It Still Goes Unreported
by Jenn Lukens
 Tucked away in the foothills of
the Blue Mountains in northeast Oregon, Grande Ronde
Hospital seemed like a safe place to Elaine LaRochelle,
CHFM and Director of Facilities. "When I
started here 19 years ago, we didn't lock any of our
doors. We were an open facility 24/7," she
recalled.
Tucked away in the foothills of
the Blue Mountains in northeast Oregon, Grande Ronde
Hospital seemed like a safe place to Elaine LaRochelle,
CHFM and Director of Facilities. "When I
started here 19 years ago, we didn't lock any of our
doors. We were an open facility 24/7," she
recalled.
A few years ago, she noticed a change. What has been referred to as an "epidemic" or a "public health challenge" found its way inside their walls: Violence against healthcare workers was no longer isolated to a select few patients experiencing dementia or mental health issues in the Critical Access Hospital's intensive care unit.
"We didn't know what to do. We have big problems the cities were having, but we just have singular events rather than a constant stream of them. We're dealing with the same folks, it's just one at a time," said LaRochelle.

With the rise of opioid use across the nation, Grande Ronde staff have seen some of the effects dependency can have inside hospitals. "When they don't get their prescription, the people that take the brunt are our front-desk staff — usually 20-something young gals — and they don't know how to cope with that. They are supposed to be customer service, and here's this customer screaming and yelling and making threats," LaRochelle shared.
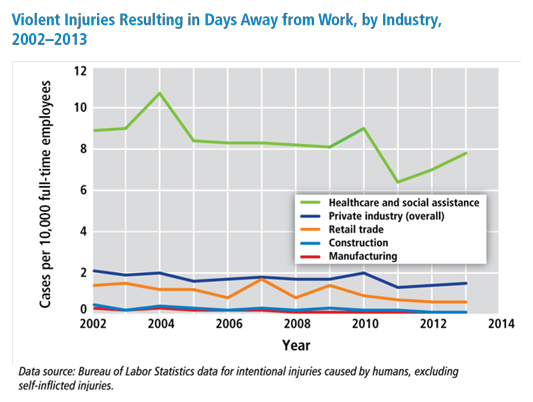
When conversation centers around violence in communities, the tendency is to associate healthcare workforce with treating the victims, not being the victims. According to the Occupational Safety and Health Administration (OSHA), healthcare and social assistance workers are four times more likely to be seriously injured by violence on the job than other professionals. The growing spotlight on the issue has identified characteristics of violence against healthcare workers, the problem of underreporting, and the positive effect rural workplace violence (WPV) initiatives can have on preventing and mitigating violence.
Characteristics of Workplace Violence Against Healthcare Workers

Dr. Judith Arnetz, PhD, MPH, PT, Associate Chair for the Research Department of Family Medicine at Michigan State University, has studied patient-to-worker violence as a lead researcher on the topic. Her 2015 study identified that the most common risk factors that induce violence include extreme pain, the use of needles, and patients who have to wait or be transferred. "These conditions can lead to violent behavior anywhere," said Arnetz. But it's the healthcare workforce that end up getting the brunt of it.
Research shows that 80% of all violence-related injury in healthcare workers comes from patients. This patient-to-worker violence is also known as Type II violence and tends to be directed toward nurses and aides — those who are on the frontline of delivering care.
An altered state of mind influenced by dementia, delirium, substance use, and mental health is another major factor. Kevin McEwan, MSN, RN, is the Chief Nursing Officer at Madison Memorial Hospital in rural Rexburg, Idaho. Nearly half of the patients treated by his nurses in the intensive care unit (ICU) suffer from some degree of delirium (within the elderly population, that goes up to almost 70%). The nature of their illness explains why: an altered state of mind could be caused by a number of factors, including severe illness, pain, medication, infection, surgery, or substance use, to name a few. The effects can produce uncharacteristic behaviors in patients.

"Family members say they have never seen their loved ones like that, that this [behavior] is unique," explained McEwan. "One moment they are fine, and the next, they are pulling on tubes and wires and the nurses are trying to control them, and the kicking, spitting, and biting all occurs just because they are confused. It's not because they are usually combative or difficult."
But physical displays are not the only forms of WPV that cause harm. Results from another of Arnetz's studies found verbal aggression to be the highest reported form of violence toward healthcare workers. "It may not be as severe — in other words it may not result in physical harm — but in interview studies, employees have said to us that it's actually the nonphysical violence that is the most difficult to deal with because it's ongoing; it's every day."
Arnetz's background as a physical therapist serving patients with special needs helps her empathize: "To have patients and their family members yell at you, curse at you, threaten you — it's demoralizing and it makes it difficult in the long run to maintain the compassion that you want to maintain as a healthcare provider."
Those from whom McEwan and his staff see the most violence are behavioral health patients. With no psychiatric unit in their rural hospital and limited psychiatric beds across the state, patients needing careful watch are kept in the ER or admitted to the ICU or a hospital room for observation until they can be sent to a facility that can meet their needs.
There are ways to help put patients at ease and deescalate volatile situations that healthcare leaders can teach staff. McEwan started WPV training for all ICU, ER, house, and nursing staff, teaching them to deploy simple steps to calm patients, like reorienting them, redirecting them to familiar items, or inviting a loved one in the room. Medication is generally administered as a last resort. "It's not that we can't give them medication to help with that anxiety, but we try not to because they are already on so many medications," explained McEwan.
Changing the Perception — Violence is "Not Okay"
While proximity, nature of care, and time spent with patients make nurses and nursing assistants more prone to violence from patients, it's the tolerance of violence that needs to be reevaluated.
That is actually a big part of the workplace violence problem — healthcare workers don't necessarily condone the violence, but they say, 'Well, the patient really didn't know what they were doing. It wasn't intentional.'
"That is actually a big part of the workplace violence problem — healthcare workers don't necessarily condone the violence, but they say, 'Well, the patient really didn't know what they were doing. It wasn't intentional.' That very well may be true, but that doesn't solve the problem or help the problem to have that attitude," agreed Arnetz.
A 2017 study conducted by Arnetz took the reality of underreporting of violent events into careful consideration in the first ever large-scale randomized controlled intervention that was effective in reducing violence toward healthcare workers. The data-driven study was conducted within a Michigan health system. Arnetz and her team helped unit supervisors pinpoint risk factors for violence and create an action plan with unit staff using a checklist of strategies. After six months, violent events were found to be significantly lower among these units, and violence-related injuries decreased at the end of a two-year period.
LaRochelle has seen underreporting play out with her colleagues and attributes it to two factors: First, some seasoned nurses have the mindset that taking a hit is just "part of the job." Second, with so many demands on their time, they don't always take the time necessary to report it.

Because early education and mentoring can play a critical role in culture change, Grande Ronde has partnered with Oregon Health & Science University School of Nursing to help instructors include WPV training into their curriculum. LaRochelle has noticed that newer nurses have been equipped and are more likely to report incidents and call for backup.
Although underreporting is still being worked on at Grande Ronde Hospital, reports have improved since the start of WPV prevention efforts, from an estimated 90% of incidents going unreported to about 50%.
One of the conclusions drawn from Arnetz's studies is the important place that violence prevention climate (a validated measure by researchers) has in a hospital setting. The environment and work conditions as well as an emphasis on teamwork and support from management can make all the difference in a healthcare worker feeling — and being — safe.
McEwan has taken violence prevention climate seriously when dealing with the ICU and emergency room nurses who have reported to him for the past 20 years: "I believe in listening to our frontline," he said. He personally follows up with every violent incident report within days, engaging the hospital's social workers for a debrief about the incident and a review of what could have been done differently. A final and important step McEwan takes is showing appreciation to those who reported so they are encouraged to do so again.
Hospitals Take a Stand Against Violence
 The American Hospital Association (AHA) has
engaged in the WPV conversation. Their Hospitals
Against Violence: Workforce and Workplace Violence
initiative is a platform for hospitals across the
nation to take action. The initiative's resources,
case studies, and
developing research have served as guides to
hospital policies and informed new initiatives. AHA's
national campaign #HAVhope
Friday: Day of Awareness every June is a way for
hospitals to publicly stand against workplace violence.
Hospitals have used the day to conduct press
conferences, hold trainings for violence prevention, or
run social media campaigns.
The American Hospital Association (AHA) has
engaged in the WPV conversation. Their Hospitals
Against Violence: Workforce and Workplace Violence
initiative is a platform for hospitals across the
nation to take action. The initiative's resources,
case studies, and
developing research have served as guides to
hospital policies and informed new initiatives. AHA's
national campaign #HAVhope
Friday: Day of Awareness every June is a way for
hospitals to publicly stand against workplace violence.
Hospitals have used the day to conduct press
conferences, hold trainings for violence prevention, or
run social media campaigns.
Creating a Workplace Safety Initiative
According to an American Hospital Association research report, hospital violence involving a staff member can have significant financial ramifications, from expenses associated with staff turnover to medical care required. However, an even bigger share — over 40% of the cost of violence to U.S. hospitals — is related to prevention and preparedness. Because of that, creating an effective action plan is important to getting a greater return on that investment.

Katie Harris, MPH, is the Director of Rural Health and Federal Policy at the Oregon Association of Hospitals and Healthcare Systems (OAHHS). She oversees the Workplace Safety Initiative (WSI) that launched a workplace violence prevention pilot project in 2014 involving five hospitals (four from rural) across different parts of the state. At the time, there weren't many comprehensive resources.
"We really needed to build and pilot a lot of tools because they weren't there," said Harris. They used the pilot project to inform an extensive Toolkit for Prevention and Management, a free guide to developing WPV initiatives. The toolkit has been identified by the Joint Commission as a credible resource for healthcare leadership, committees, and stakeholders.
Some of the pilot sites already had a WPV initiative but others, like Grande Ronde Hospital, did not.
LaRochelle was approached by Grande Ronde's CEO to run the OAHHS pilot program. As her role encompasses safety and security of staff, it seemed like a natural fit. Because the state of Oregon requires that WPV initiatives have a committee, the first thing LaRochelle did was form a multi-disciplinary team of management and staff, including representatives from nursing, quality and risk management, human resources, and facilities.
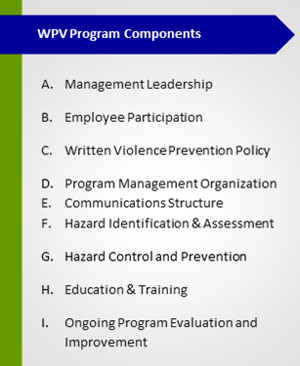
After identifying vulnerable areas by using the WSI gap analysis tool, the Grande Ronde team put a plan together. They started small with simple changes like installing locks on the lobby door, then moved to bigger goals like creating a WPV policy. After a trial run in the ICU proved successful, the committee applied their plan throughout the entire facility. Each time they tried something new, LaRochelle would share it with other pilot sites at quarterly meetings.
Harris said that, throughout the course of creating the toolkit, making it realistic for rural hospitals to use was at the forefront of their minds: "We didn't want people to have to hire an outside consultant to do this work, because we know it's just not feasible and it's just one more thing, one more project."
So, they created the toolkit to be used piece by piece, with core elements for hospitals to consider, scalable steps, and links to individual sections and tools. An editable version allows hospitals to cater it to fit the needs of their facility.
Because hospitals in Oregon are now required by law to have a WPV initiative, all 62 have used the toolkit in some way. Harris's biggest advice to them and others is to start small. "Try a mini-pilot in one area of the facility; try to roll something out within just one unit. I think this is especially helpful for a rural hospital that has fewer resources. This is a way to play with some ideas without having to totally invest in something one hundred percent."
A Toolkit for Nurse Leaders
Kevin McEwan is on the board of the American Organization for Nursing Leadership (AONL), a subsidiary of the American Hospital Association. Along with the Emergency Nurses Association, AONL has developed the Toolkit for Mitigating Violence in the Workplace for nurse leaders. It outlines six essential steps to address workplace violence that McEwan has enacted at Madison Memorial Hospital:
- Understand workplace violence
- Develop a zero-tolerance policy
- Assess the risk factors in your facility
- Develop a workplace violence prevention plan
- Train and deploy staff
- Evaluate the changes and identify next steps
Challenges and Advantages to Addressing WPV in Rural Hospitals
While research focused on WPV in rural hospital settings is limited in the United States, researchers and practitioners agree that, although the type of violence is similar in urban facilities, the method in which it is addressed — or prevented — can differ.
Take hospital infrastructure. The 2011 Emergency Department Violence Surveillance Study (no longer available online) conducted by the ENA found that the greatest risk of violence in healthcare facilities occurs in patient rooms, then corridors, halls, stairwells, and elevators. When money is tight (a reality for many rural hospitals), upgrades for infrastructure improvements that could help with security in these locations — like adding more windows to improve lighting, widening hallways, and creating more entry and exit points — can get put on the backburner.
LaRochelle oversaw recommended facility upgrades as part of the pilot project, like the conversion of the hospital admission stations to standing desks to put clerks at eye-level with patients, reducing the opportunity for intimidation. A full-time security guard is now stationed in rooms of patients who have shown violent tendencies, and a system that controls the elevators from the nurse's station after hours adds to the security upgrades throughout the facility.
External communication is also important for rural hospitals starting a WPV initiative. A close relationship with the local police station gets backup to Madison Memorial Hospital's ER within minutes when called. Fluid internal communication at Grande Ronde Hospital helps staff across all departments stay informed. For instance, a patient's electronic medical record (EMR) can be flagged to indicate violent tendencies, but since not every staff member has access to the EMR, a magnet strategically placed on the patient's door frame is used as a signal to staff to be extra cautious. When deployed, a "code gray" is an indicator that a hospital staff member needs assistance with a patient. These small steps have helped increase awareness and, LaRochelle believes, dodged violent incidents before they begin.
The benefits to being small and rural is that we know those people more likely to be violent, and we know how to deal with them most effectively.
According to McEwan, familiarity with patients is an especially helpful advantage when treating those with behavioral health conditions prone to violent behavior. "The cyclical nature of behavioral health — whether inpatient psych or local ER — there seems to be some repetition," he explained. "The benefits to being small and rural is that we know those people more likely to be violent, and we know how to deal with them most effectively."
Madison Memorial Hospital used to send a "Notice of Dire Need" to patients who have exhibited violent behavior, stating that admittance will not be permitted unless there is a critical emergency. "But that's hard to do in a small community because you are often THE hospital, so you can't really tell a patient to not come back because they've had some bad behaviors last visit," said McEwan.

They adjusted the process and now Madison Memorial Hospital's social worker and management team work with the patient and their family to develop an individualized care plan for these patients, outlining behaviors that will not be tolerated. McEwan reported that it works well for some, and others need additional action steps, "but at least we have some ground rules."
The changes made to Grande Ronde Hospital's response to violent incidents have made an impact on their frontline staff. LaRochelle shared, "In the past, we've had staff quit, saying 'I'm tired of getting beat up. I wanted to be a nurse, not a combat vet.'" One of the nurses who had left because of the work conditions returned last year because "she feels like now she can work here."
To LaRochelle, the four-year process of rolling out WPV interventions to create a culture of safety for this nurse and other staff was worth it: "They feel we listened. They feel we did something, and they feel safer being at their jobs."
Additional Resources
- Preventing Workplace Violence in Healthcare, Occupational Safety and Health Administration (OSHA)
- Violence Occupational Hazards in Hospitals, The National Institute for Occupational Safety and Health (NIOSH)
- Workplace Violence against Health Care Workers in the United States, The New England Journal of Medicine
- Workplace Violence Prevention for Nurses, The Centers for Disease Control and Prevention (CDC)
- Workplace Violence Prevention Resources for Health Care, The Joint Commission
- Workplace Violence Resources and Education, Emergency Nurses Association (ENA)
- The International Association for Healthcare Security & Safety offers journal articles, at-risk patient screening information, and training and certifications.
