Facing Diabetes: Quality Improvement in Rural South Dakota Project
- Need: To help adults and children in rural South Dakota prevent or manage their diabetes.
- Intervention: The Facing Diabetes Project offered medical visits for adults and provided prevention and education sessions for the local 4th and 5th graders.
- Results: Many adults and children in the region felt better equipped to choose healthy foods, exercise regularly, and manage their stress: all factors that can help prevent diabetes or decrease its effects.
Description
The rural counties of Charles Mix, Douglas, and Hutchinson in southeastern South Dakota face high rates of smoking, drinking, unhealthy eating, and physical inactivity. In addition, the three counties are considered Medically Underserved Areas and Health Professional Shortage Areas in primary care, potentially preventing those with chronic conditions from receiving the quality care they need. Due to these factors of unhealthy lifestyles and limited access to health professionals, many adults and children in the region find it difficult to manage their diabetes or prevent it.
Avera St. Benedict Health Center in rural Parkston has over 300 patients with diabetes in its service area. Avera St. Benedict began a pilot program of group medical visits, where community members could meet as a group and work with a dietitian, behavioral health specialist, and nurse practitioner. The pilot program of the Facing Diabetes Project had 65 people.
Avera St. Benedict partnered with the Andes Central School District, the Parkston Ministerial Association, and the Parkston School District. The community-wide effort helped participants receive care and support from the many organizations in their lives. Patients could get referred in from anywhere; they did not need a doctor's note in order to participate in the group medical visits.
This project received support from a 2013-2016 Federal Office of Rural Health Policy (FORHP) Small Health Care Provider Quality Improvement grant and was able to offer group diabetes care to all Avera St. Benedict patients with diabetes.
The services from this grant period have ended. The following services, which cover chronic diseases in general, are offered:
- The Colony Outreach Nurse provides diabetes education to Hutterite Colony members on an individual basis or in small groups.
- Four staff members are trained in Better Choices, Better Health® (BCBH) to provide the original BCBH curriculum, a diabetes-specific BCBH, and a chronic pain BCBH. These programs have replaced the FORHP-funded diabetes groups.
- Patients can request a joint visit from a dietitian and nurse practitioner.
- The clinics in Parkston, Lake Andes, and Tripp have a chronic care management (CCM) nurse, care coordinator, health coach, and behavioral health team for CCM services, South Dakota Medicaid Health Home services, and care coordination services for Medicare patients.
Services offered
The Diabetes Care Team provided specialized education and management support to community members with or at risk of diabetes. The team consisted of a behavioral health specialist, a dietitian, and a diabetes educator/nurse practitioner.
Adults with diabetes or prediabetes could participate in group medical visits, which later became individual visits. During these visits, providers checked their patients' vitals and made sure they were up to date on:
- Medications
- Lab work
- Foot exams
- Neuropathy eye appointments
After the initial checkup, patients and providers had a conversation about a patient-chosen topic. Topics included:
- Portion size
- Carb counting
- Stress management
- Insomnia treatment
- Smoking cessation
Other topics were even more patient-driven, as groups discussed how to find healthy foods when traveling, what to eat at a potluck, or how to barbecue foods in a healthier way. Patient-driven topics allowed the group medical visits to be more practical for the patients, as they voiced any struggles with their management and offered tips to their fellow group members.
The Facing Diabetes Project also worked with members of the Yankton Sioux Tribe and the nearby Hutterite Colonies. While the group format and many of the discussion topics were the same, staff leaders could adjust the Facing Diabetes Project to better meet the specific needs of a community. For example, those living in the Tschetter Colony eat their meals communally, so discussion topics focused more so on portion control and healthy snacks than on meal preparation. Group medical visits also took place in the Colonies and at Avera St. Benedict Certified Rural Health Clinic in Lake Andes, located on the reservation, so these patients didn't have to travel.
Individual sessions provided access to a dietitian and behavioral health specialist along with the primary care provider, and sessions covered many of the same topics as the previous group visits. Staff members also traveled to worksites for employees unable or unwilling to leave work in order to see a doctor. Employees, often in agribusiness, had their blood pressure, lipids, and glycated hemoglobin (HbA1c) rates checked.
Fourth and fifth graders in the region, including those from the Colonies, participated in prevention and education sessions at their schools. The activity-based sessions took place in the gym with the help of the local P.E. teachers. Many of the topics, like exercise, healthy eating, and mood management, were similar to those in the adult classes. Other topics included diabetes prevention and consequences of diabetes.
Results
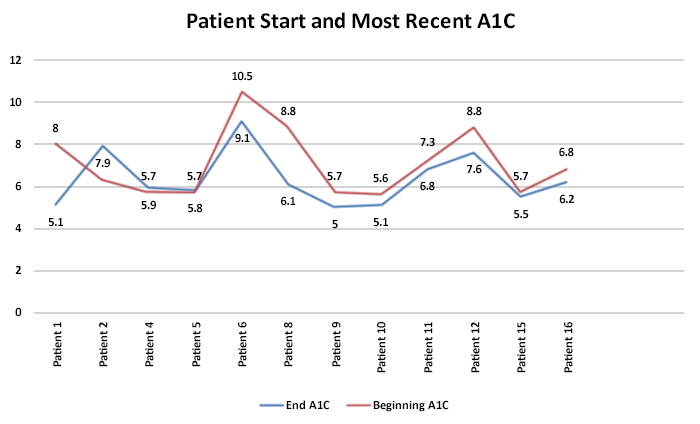
Patients completed questionnaires and had their vitals measured before and after participation in the program. Participants showed improvement in body mass index (BMI), HbA1c rates, blood pressure, and stress levels. Participants also reported excellent satisfaction with the sessions and improved knowledge of nutrition, exercise, and diabetes monitoring:
- 86% of the first-year respondents (2013-14) and 89% of the second-year respondents (2014-15) said they would recommend the program to others
- 100% of first-year and 89% of second-year respondents said that their questions about diabetes management were answered and that the information was practical and clearly explained
- 100% of first-year and 71% of second-year respondents felt confident in being able to manage their diabetes
- 90.1% of the 4th and 5th graders surveyed said they learned new facts about healthy eating
- 88.6% of the 4th and 5th graders said they learned the importance of regular exercise
- 78.9% of the 4th and 5th graders said they learned how to manage their moods
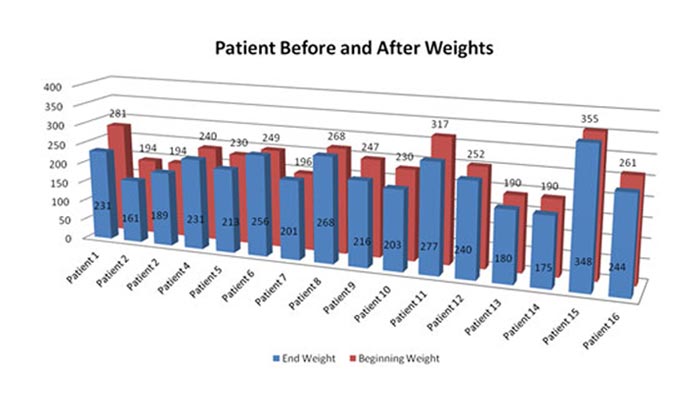
In 2013-14, 35 Parkston patients and 14 Lake Andes patients participated in group or individual sessions. In 2014-15, 25 Parkston patients, 79 Lake Andes patients, and 15 Tschetter Colony patients participated in group or individual sessions.
In 2015:
- 90 adults received services from group or individual interventions with the diabetes team
- 99 employees were screened at their worksites
- 108 children were educated at the Parkston and Andes Central school districts
Challenges
At times, the rural lifestyle and weather could be a barrier, especially in the Dakotas. A blizzard may have taken place on Group Day, or agricultural workers may not have wanted to leave the fields during planting or harvest season. During extreme weather, staff members often called patients and told them to stay home, especially if the patient lived outside of town.
Finding what worked best for patients proved to be a trial-and-error process. Staff members kept adjusting the frequency of visits to see whether attendance would be better for monthly or biweekly visits. The Facing Diabetes Project also began with patients assigned to fixed groups but later switched to rotating groups, where patients can join any group at any time.
Traveling and school schedules proved to be a barrier as well. The Lake Andes clinic is located 50 miles from Parkston, and staff members had to travel to the Lake Andes schools several times a week in order to work with the 4th and 5th graders there. Lake Andes and Parkston schools sometimes have different schedules, which can make event planning difficult.
Replication
Be patient and willing to adjust the project until it's successful. The project is not hugely revenue-generating at first, and each facility will have different groups of patients with individual schedules and needs. The Facing Diabetes Project worked best when clinics had people who could invest time into making the project work and would listen to patients' comments or concerns.
Not every area will have a dietitian or behavioral health specialist on staff. If unable to hire new staff, you can make the project work with your current staff, since many will already have knowledge of healthy eating. For example, the diabetes educator/registered nurse at Avera St. Benedict resigned, so a nurse practitioner was asked to step in. Really small healthcare facilities may even be able to run a project similar to the Facing Diabetes Project with a nurse and an advanced practice provider.
Contact Information
Lindsay Weber, CNP, President/CEOAvera St. Benedict Health Center
605.928.3311 Ext. 75264
Lindsay.Weber@avera.org
Topics
Anabaptists
· Children and youth
· Chronic disease management
· Diabetes
· Tribal communities
States served
South Dakota
Date added
June 21, 2016
Suggested citation: Rural Health Information Hub, 2023. Facing Diabetes: Quality Improvement in Rural South Dakota Project [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/910 [Accessed 9 October 2025]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
