Community Care Partnership of Maine Accountable Care Organization
- Need: To increase access and quality of care for patients in rural Maine.
- Intervention: Community hospitals and Federally Qualified Health Centers in Maine formed the Community Care Partnership of Maine Accountable Care Organization (CCPM ACO).
- Results: CCPM serves about 120,000 patients in Maine. In addition, it has implemented shared savings arrangements/contracts with different Medicare Advantage and other private health payers.
Description
The Community Care Partnership of Maine Accountable Care Organization (CCPM ACO) began in August 2015 and became a Medicare Shared Savings Program ACO in January 2016. The ACO began when Penobscot Community Health Care (PCHC) and St. Joseph Healthcare in Bangor partnered together. This Federally Qualified Health Center (FQHC) and community hospital, respectively, then invited rural community health centers and community hospitals to join.
While collaborating with major healthcare facilities in Bangor and Portland, the rural facilities in this ACO still maintain independence. Each member organization is considered a joint owner in CCPM and receives one vote in decision-making, whatever the organization's size.
The participating hospitals are:
- Cary Medical Center
- Millinocket Regional Hospital
- Mount Desert Island Hospital
- St. Joseph Healthcare
The participating FQHCs are:
- Bucksport Regional Health Center
- Community Clinical Services, Inc.
- Eastport Health Care, Inc.
- Fish River Rural Health
- Greater Portland Health
- Harrington Family Health Center
- Health Access Network
- HealthReach Community Health Centers
- Hometown Health Center
- Islands Community Medical Services, Inc.
- Katahdin Valley Health Center
- Nasson Health Care
- Pines Health Services
- Regional Medical Center at Lubec
- Sacopee Valley Health Center
- St. Croix Regional Family Health Center
Through one of its member organizations, CCPM was awarded a 2016-2019 Federal Office of Rural Health Policy (FORHP) Small Health Care Provider Quality Improvement grant. In 2021, CCPM secured more than $1 million in funding to support several of its initiatives, including comprehensive pre-visit planning, diabetes prevention, and early detection of lung cancer.
Services offered
CCPM uses a health information exchange (HIE) called HealthInfoNet to share patient information among the hospitals and FQHCs. This HIE allows the facilities to provide better-coordinated care to their patients and to collect population health data. In addition, the HIE provides real-time predictive analytics in order to predict (and work to prevent) readmissions. CCPM is working to incorporate social determinants data from two regional community action programs.
CCPM also allows member organizations to share services in order to reduce costs and duplicated services. Rural organizations do not have to "reinvent the wheel" when they can borrow another organization's expertise or services.

CCPM is a forum for sharing best practices on how to help patients be as healthy as possible and how to help reduce unnecessary emergency department visits or hospitalizations. Rural member organizations particularly like how monthly sharing with their peers reduces rural isolation and provides collegial support.
CCPM hosts a series of recurring meetings where members convene to discuss changes and innovations in patient care, quality, and data analytics. These include Quality & Clinical Integration, Care Management, and Medical Directors meetings.
In 2019, CCPM launched Pharmacy Consults as a benefit of ACO membership. Any patient of its 21 member organizations is eligible to receive this service. CCPM employs a Clinical Pharmacist to support this service line. Upon referral, the Clinical Pharmacist performs a comprehensive medication review and issues recommendations that include:
- Changes in the medication regimen
- Instructions for monitoring for specific desired (or undesired) outcomes
- Suggestions for management of potentially inappropriate medication use
In 2019, CCPM began onboarding and training medical assistants (MAs) to support its member organizations with pre-visit planning. CCPM's centralized MAs are specially trained to provide comprehensive pre-visit planning, reducing administrative burden and freeing up time for both the provider and MA. CCPM's pre-visit planning MAs now serve 10 of the 21 member organizations and are working to operationalize the service with additional organizations.
CCPM offers medication-assisted treatment (MAT) and care management consultation on a contracted basis to interested member organizations. In addition, CCPM offers a free online Continuing Medical Education (CME) Series as a benefit of ACO membership. Any employee of the 21 member organizations is eligible to access the library of AMA-accredited CME modules, many of which are tailored to an FQHC audience.
Results
Over the course of several years, CCPM has implemented a complex LLC legal structure, compliance program, organization, and financial structure. CCPM also covers about 120,000 patients in Maine.
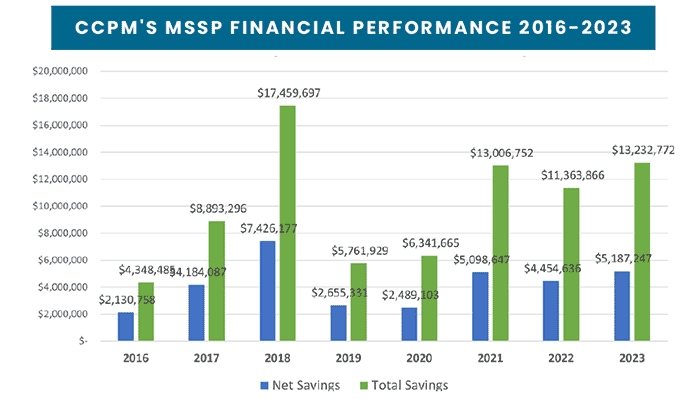
CCPM has earned shared savings for 8 consecutive years under the Medicare Shared Savings Program (MSSP). In addition, CCPM has implemented shared savings arrangements/contracts with different Medicare Advantage and other private health payers.
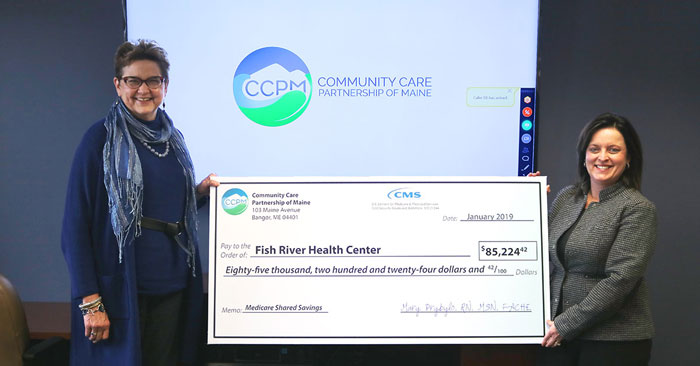
In 2016, CCPM had a savings of $4.3 million in the MSSP. In 2017, this savings was over $8.8 million. In 2018, CCPM generated over $17.2 million in savings under the MSSP, resulting in about $7.4 million shared savings for CCPM, which was then distributed back to its participating member organizations. This success continued in 2019, 2020, 2021, and 2022. Most recently, in 2023, CCPM generated over $13.2 million in savings under MSSP, resulting in about $5.1 million in shared savings for CCPM. CCPM is the only ACO in Maine, and one of a handful of ACOs nationwide, to have achieved shared savings for 8 consecutive years (2016-2023).
The ACO was named a 2016 Case Study in Innovation by the American Hospital Association and presented its work at the AHA Rural Health Care Leadership Conference in February 2017.
Challenges
While CCPM views its vast geography spread across the state as a strength, it recognizes that the distance poses some logistical barriers. To overcome these barriers, CCPM hosts the majority of its committee meetings virtually to reduce travel time for attendees, a practice that allowed it to continue operations during the COVID-19 pandemic.
CCPM also contends with the use of multiple electronic medical records (EMRs) across its 21 member organizations, which at times poses challenges in starting new initiatives.
Replication
Some member organizations had tried other ACO models but felt that they didn't "fit" into these work cultures. CCPM was a better fit because the member organizations shared similar values, like focusing on their communities' immediate needs.
CCPM also credits its long-standing success to the leanness of its organizational structure. All of CCPM's officers fulfill their role in a part-time capacity while also serving in a separate role at one of its member organizations.
Contact Information
Danielle Brown, Executive AdministratorCommunity Care Partnership of Maine
daniellebrown@ccpmaine.org
Topics
Accountable Care Organizations
· Federally Qualified Health Centers
· Healthcare quality
· Hospitals
· Primary care
States served
Maine
Date added
February 17, 2017
Suggested citation: Rural Health Information Hub, 2025 . Community Care Partnership of Maine Accountable Care Organization [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/944 [Accessed 6 March 2026]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
