Project ENABLE (Educate, Nurture, Advise, Before Life Ends)
- Need: To enhance palliative care access to rural patients with serious illness, such as advanced cancer, heart failure, and COPD, and their family caregivers.
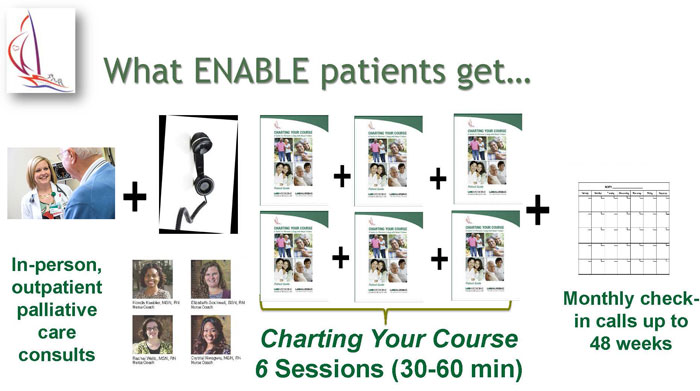
- Intervention: Project ENABLE consists of: 1) an initial in-person palliative care consultation with a specialty-trained provider and 2) a semi-structured series of weekly, phone-delivered, nurse-led or palliative care coach/navigator sessions designed to help patients and their caregivers enhance their problem-solving, symptom management, and coping skills.
- Results: Patients and caregivers report higher quality of life and lower rates of depression and (caregiver) burden.
Evidence-level
Evidence-Based (About evidence-level criteria)Description
 Palliative care is often limited in
resource-scarce rural communities. While palliative care
has traditionally been offered only after exhausting
curative treatment options, a growing number of clinical
trials demonstrate that offering palliative
care at the time of diagnosis and concurrent with
disease-oriented care can help improve patients'
symptoms, quality of life, and mood and help them and
their caregivers plan for an unpredictable future.
Palliative care is often limited in
resource-scarce rural communities. While palliative care
has traditionally been offered only after exhausting
curative treatment options, a growing number of clinical
trials demonstrate that offering palliative
care at the time of diagnosis and concurrent with
disease-oriented care can help improve patients'
symptoms, quality of life, and mood and help them and
their caregivers plan for an unpredictable future.
Project ENABLE (Educate, Nurture, Advise, Before Life Ends) is a telehealth approach that provides palliative care to patients with serious illnesses and their family caregivers. ENABLE was developed in rural New Hampshire and Vermont and is now being implemented and tested across the United States and in selected areas of Honduras, Iran, and Turkey and Singapore.
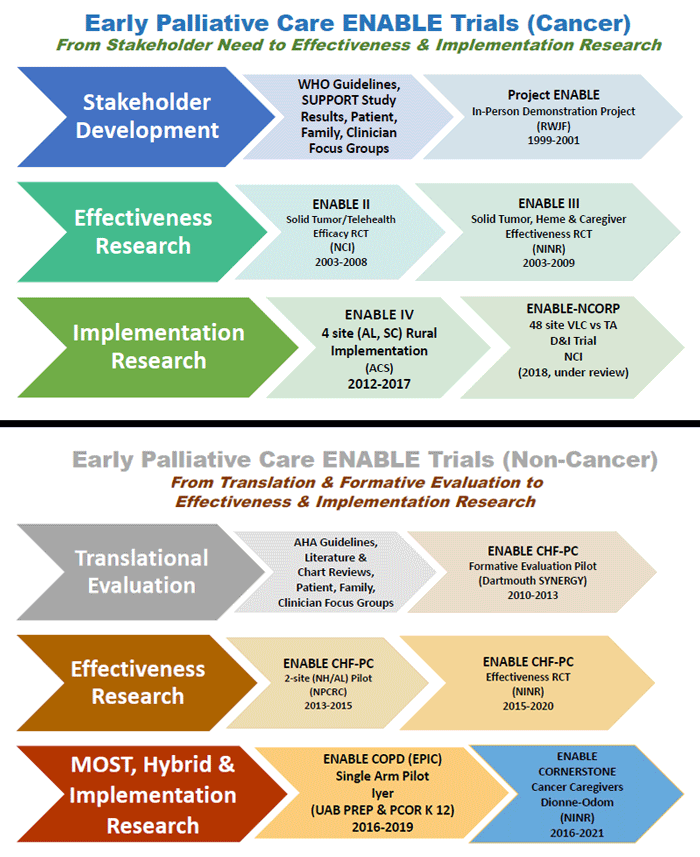
History of Project ENABLE
Project ENABLE I (1998-2001) was developed through a Robert Wood Johnson Foundation-funded demonstration project involving 380 patients at three northern New Hampshire cancer practices: the Norris Cotton Cancer Center (NCCC) at Dartmouth Hitchcock Medical Center in rural Lebanon, Oncology Associates in Manchester, and a Critical Access Hospital in rural Berlin. The goals were to provide a supportive care intervention to patients who were newly diagnosed with advanced cancer and had limited access to palliative care.
A nurse coach met with patients to facilitate a 4-session seminar guided by the Charting Your Course guidebook, which helps patients and families better cope with their physical, functional, emotional, and spiritual needs. The nurse coach also coordinated care between the cancer centers and their communities. Family caregivers were invited but not required to attend. If they were interested but unable to attend in person, nurse coaches provided the content to patients and families over the phone.
ENABLE II (2003-2008) was a randomized controlled trial (RCT) funded by the National Cancer Institute (NCI). Building on ENABLE I, including adapting the in-person intervention to one delivered by phone, the study's aim was to evaluate the efficacy of ENABLE to improve quality of life, symptoms, and mood for patients with advanced cancer compared to standard care. Over 300 patients enrolled over 4 years: Half of the patients received ENABLE and half received usual cancer care. Family caregivers did not receive a specific intervention but were invited to participate in patients' in-person palliative care consultations.
ENABLE III (2010-2013), funded by the National Institute of Nursing Research (NINR), was an RCT examining the timing of providing ENABLE to patients and a parallel intervention for family caregivers. Patients and their caregivers were randomly assigned to receive the intervention immediately or 12 weeks after enrollment. The intervention included an in-person comprehensive assessment by a palliative care-certified clinician followed by nurse coach-delivered telehealth sessions. (Patients received 6 sessions and caregivers received 3 sessions.) The patient and caregiver each had a different nurse so that each participant could share questions or concerns freely. Nurses maintained monthly contact with patients and caregivers after the sessions were completed.
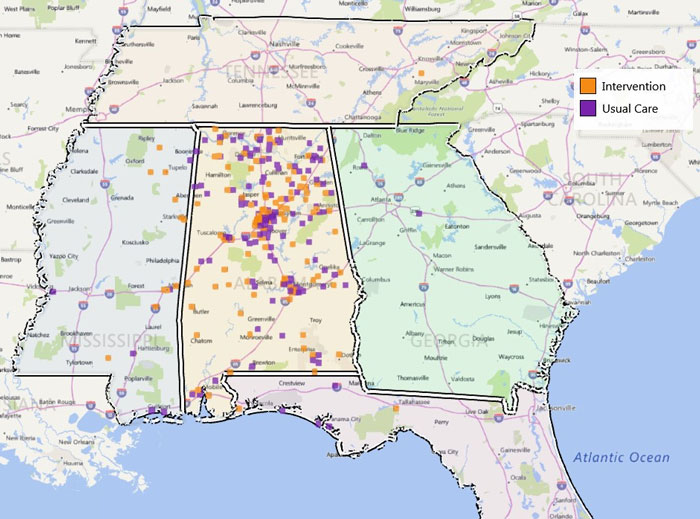
ENABLE IV (2012-2017), funded by the American Cancer Society, was an implementation science study using a virtual learning collaborative (VLC) approach to implement ENABLE at rural-serving community cancer centers in Alabama and South Carolina. ENABLE implementation teams at each site were supported by University of Alabama at Birmingham Coordinating Center experts via monthly videoconferences and annual site visits. Site teams reported monthly progress, patient experience, implementation costs, and lessons learned.
ENABLE CHF-PC (Comprehensive Heartcare for Patients and Caregivers: 2010-2020), funded by Dartmouth SYNERGY, the National Palliative Care Research Center pilot awards, and NINR, adapted ENABLE to also serve patients with heart failure and their family caregivers. ENABLE CHF-PC combines an in-person palliative consultation by a palliative care specialist and weekly nurse coach telehealth sessions (6 for patients and 4 for caregivers) and monthly follow-up. The sessions also follow "Charting Your Course," and services are tailored to meet a patient's and family's unique needs.
ENABLE V (2018-2023), an NCI-funded implementation trial, compared the effectiveness of VLC versus technical assistance on ENABLE program uptake as measured by the proportion of patients at 48 participating NCI Community Oncology Research Program (NCORP) practices across the country. The long-term goal was to generate knowledge about ways to improve the adoption, adaptation, integration, and scalability of evidence-based practices and to improve the integration of ENABLE in oncology practices to reduce disparities for patients.
ENABLE-CORNERSTONE (2017-present), funded by a NINR R00 pilot award and now by NCI, is a hybrid type I randomized effectiveness-implementation trial with 212 advanced cancer family caregivers in the South to assess a lay navigator-led intervention of 6 brief, weekly in-person/telephone sessions followed by monthly follow-up every 4 weeks as needed.
ENABLE-EPIC (Early Palliative Care in COPD) (2018-present) – now Empowering People with Independence in COPD (2023-present) – funded by the Agency for Healthcare Research and Quality (AHRQ), a University of Alabama at Birmingham Palliative Research Enhancement Project Award, and the National Institute on Aging, is a series of pilot trials to translate and test ENABLE for a population with chronic obstructive pulmonary disease (COPD). The purpose of this study is to explore the impact of an ENABLE-informed weekly phone coaching program on independence, mobility, well-being, and symptoms for people living with chronic obstructive pulmonary disease.
ENABLE LVAD (Left Ventricular Assist Device) (2018-2023) was a Patient-Centered Outcomes Research Institute-funded implementation project expanding shared decision-making programs and resources to support individuals with a LVAD and their family caregivers. The ENABLE "Charting Your Course" guidebook was adapted for clinician and caregiver use, and materials like user manuals and training webinars were available for staff.
Project UPHOLDS (2021-2025), a NINR-funded optimization pilot informed by ENABLE CHF-PC, is a two-phase trial to adapt, refine, and optimize early palliative care intervention components and levels for older adults living with advanced heart failure. After a formative evaluation (2021-2023), ENABLE-informed intervention components were expanded to include delivery by trained palliative care coaches and content on sleep and financial distress. Pilot testing is currently underway with 64 participants to inform the optimal combination of components and levels ("doses") that most effectively and efficiently improves quality of life.
Services offered
Nurse coaches or community-based palliative care coaches provide a comprehensive palliative care assessment and palliative care coaching/psychoeducation sessions for patients and caregivers. These sessions cover topics such as symptom management, self-care, decision-making, and advance care planning. While palliative care services are considered standardized, they can be tailored to meet the individual patient's and caregiver's needs.
Results
ENABLE I:
- Compared to national and regional data, a larger number of participants in ENABLE died in their preferred site. (For many participants, this meant dying in their own home.)
- A higher percentage of ENABLE family members reported that the patient and providers worked to ensure that patient preferences for medical treatment were followed.
ENABLE II:
- Intervention patients reported lower depressed mood and higher quality of life, with trends toward improved symptom management and survival.
- ENABLE was listed as an Evidence-Based Cancer Control Program by the National Cancer Institute.
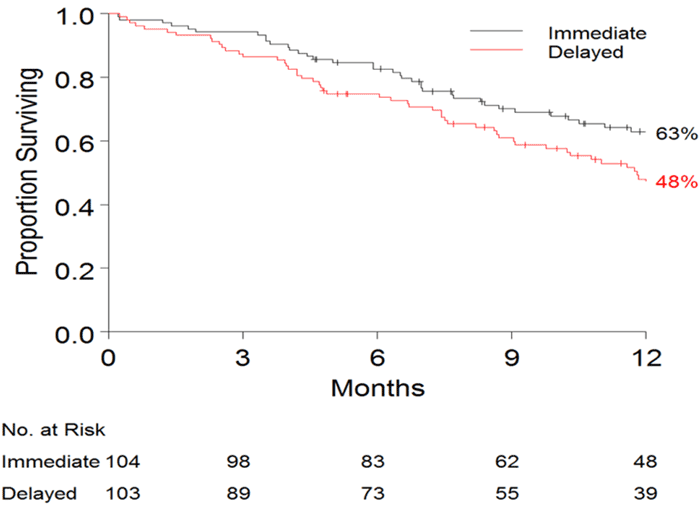
ENABLE III:
- Kaplan-Meier survival rates one year after enrollment were 63% for those in the early intervention group, compared to 48% for those who began intervention 3 months later.
- Caregivers in the early intervention group had lower depression and stress burden scores.
- The American Society of Clinical Oncology (ASCO) identified ENABLE as one of the year's greatest advances in clinical cancer care.
ENABLE IV:
- Program coordinators developed and tested the ENABLE Implementation Toolkit to assess pre- and post-implementation success.
- They demonstrated feasibility of using a VLC strategy to implement ENABLE in non-academic, community-based cancer practices that serve a high proportion of rural cancer patients and their family caregivers.
ENABLE CHF-PC:
- Results of a 2017 pilot study called "Engaging Patients and Families to Create a Feasible Clinical Trial Integrating Palliative and Heart Failure Care: Results of the ENABLE CHF-PC Pilot Clinical Trial" demonstrated feasibility of carrying out ENABLE with 61 patients and 48 caregivers in New England and the Southeast.
- Patients and caregivers experienced moderate improvements in quality of life and mental health. Patients' symptoms and physical health as well as caregivers' burden improved.
- A NINR-funded full-scale efficacy RCT enrolled 415 patients and 159 caregiver participants across the Deep South. Over 50% of participants in the trial were African American.
ENABLE-CORNERSTONE:
- 212 caregivers have been enrolled in the ongoing RCT.
ENABLE-EPIC:
- The completed formative evaluation study involved pulmonary and palliative care clinicians and 10 COPD patient/caregiver dyads.
- Preliminary pilot data demonstrates feasibility and acceptability; 37 participants have been enrolled.
- An RCT is planned.
ENABLE LVAD:
- Enrollment in the DECIDE-LVAD trial has concluded.
Project UPHOLDS:
- The completed formative evaluation study involved cardiology and palliative care clinicians, lay navigators, and adults with heart failure who provided the following recommended modifications to the ENABLE program: shorter weekly sessions (20 minutes) and information and coaching on handling financial distress and sleep issues.
- The optimization pilot is now enrolling through 2026.
For more information about Project ENABLE:
Pfahl, J., Thompson, J.S., Matlock, D.D., Allen, L.A., Dionne-Odom, J.N., Bakitas, M.A., & McIlvennan, C.K. (2024). ENABLE-LVAD: Development and Implementation of a Novel Training Program for Clinicians Supporting Family Caregivers of Patients With a Left Ventricular Assist Device. The Journal of Cardiovascular Nursing, 39(4), E136-E139. Article Abstract
Iyer, A.S., Wells, R.D., Dionne-Odom, J.N., Bechthold, A.C., Armstrong, M., Byun, J.Y., … & Bakitas, M.A. (2023). Project EPIC (Early Palliative Care In COPD): A Formative and Summative Evaluation of the EPIC Telehealth Intervention. Journal of Pain and Symptom Management, 65(4), 335-347. Article Abstract
Wells, R., Dionne-Odom, J.N., Azuero, A., Buck, H., Ejem, D., Burgio, K.L., … & Bakitas, M. (2021). Examining Adherence and Dose Effect of an Early Palliative Care Intervention for Advanced Heart Failure Patients. Journal of Pain and Symptom Management, 62(3), 471-481.
Iyer, A.S., Dionne-Odom, J.N., Ford, S.M., Crump Tims, S.L., Sockwell, E.D., Ivankova, N.V., ... & Bakitas, M.A. (2019). A Formative Evaluation of Patient and Family Caregiver Perspectives on Early Palliative Care in Chronic Obstructive Pulmonary Disease across Disease Severity. Annals of the American Thoracic Society, 16(8), 1024-1033. Article Abstract
Bakitas, M.A., Elk, R., Astin, M., Ceronsky, L., Clifford, K.N., Dionne-Odom, J.N., ... & Smith, T. (2015). Systematic Review of Palliative Care in the Rural Setting. Cancer Control, 22(4), 450-464. Article Abstract
Bakitas, M.A., Tosteson, T.D., Li, Z., Lyons, K.D., Hull, J.G., Li, Z., ... & Ahles, T.A. (2015). Early Versus Delayed Initiation of Concurrent Palliative Oncology Care: Patient Outcomes in the ENABLE III Randomized Controlled Trial. Journal of Clinical Oncology, 33(13), 1438-1445.
Dionne-Odom, J.N., Azuero, A., Lyons, K.D., Hull, J.G., Tosteson, T., Li, Z., ... & Bakitas, M.A. (2015). Benefits of Early Versus Delayed Palliative Care to Informal Family Caregivers of Patients with Advanced Cancer: Outcomes from the ENABLE III Randomized Controlled Trial. Journal of Clinical Oncology, 33(13), 1446-1452.
Challenges
Patient barriers include poverty and unemployment, level of education, mistrust of healthcare, travel to care, and insulated communities.
Clinician barriers include lack of palliative care education, experience, and expertise.
Policy/system barriers include inability of small health systems, cancer or other specialty care centers, and practices to support palliative care expertise and disincentives from limited reimbursement.
Replication
Implementation materials are available through the authors' publications and presentations. Early lessons learned from an implementation study include:
- The importance of administrative and palliative care leadership buy-in, support, and commitment
- The need for clinician champions, such as oncologists, cardiologists, and hepatologists
- Protected time for coaches to deliver the program
- The need for strategically incorporating ENABLE model elements into existing work-flow patterns
- A referral trigger that does not rely solely on clinician referral
Contact Information
Dr. Rachel Wells, Assistant ProfessorUniversity of Alabama at Birmingham School of Nursing
205.934.0962
raduncan@uab.edu
Topics
Cancer
· Cardiovascular disease
· Chronic respiratory conditions
· Hospice and palliative care
· Informal caregivers
· Telehealth
States served
National/Multi-State, Alabama, New Hampshire, Vermont
Date added
May 19, 2017
Suggested citation: Rural Health Information Hub, 2025 . Project ENABLE (Educate, Nurture, Advise, Before Life Ends) [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/956 [Accessed 19 February 2026]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.