HIV Telehealth Collaborative Care (HIV TCC) Program
- Need: To increase access to specialty care for rural veterans living with HIV.
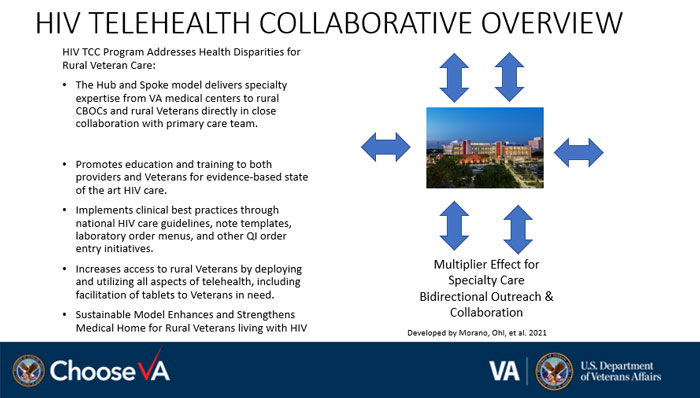
- Intervention: The HIV Telehealth Collaborative Care (TCC) study connects these patients with HIV specialists via clinical video telehealth or VA video connect and works to create shared care relationships with primary care teams in rural areas.
- Results: The HIV TCC program provides HIV specialty care access to rural veterans in a sustainable manner with infrastructure, mentorship, and capacity building.
Description
The HIV Telehealth Collaborative Care (TCC) study works to improve care for rural veterans with HIV by connecting them via telehealth services to HIV specialists in urban VA hospitals. The HIV TCC program began as a pilot at the Iowa City VA and expanded to pilots in Atlanta, Georgia, as well as Houston, Dallas, and San Antonio, Texas. The program has since expanded to include Arizona, California, Florida, Indiana, Louisiana, Maine, Mississippi, Ohio, Oregon, Tennessee, and Washington, with new outreach to Missouri completed in 2022. Outreach for 2023 is in process for Minnesota and for Hawaii for expansion to Pacific Islander patients in rural outlying islands.
Researchers received funding from VA's Office of Rural Health to develop, evaluate, and implement a program that would improve access to specialty care for rural veterans with HIV, with ongoing quality improvement work in active and sustaining sites for telehealth program sustainability.
Services offered
Patients attend their videoconferencing sessions at the nearest VA community-based outpatient clinic (CBOC) and receive care from distant HIV specialty care teams. Patients can also complete VA video connect visits in their own homes or a secure office space. Services include maintaining HIV care and ensuring associated care metrics as coordinated with the primary care provider. New services, first offered in 2022, include more comprehensive sexually transmitted infection (STI) screening in HIV care as well as more integrated services with primary care for STI treatment and prevention within HIV care.
In addition, local primary care teams in rural areas work with HIV specialists at the centrally located hub to provide "shared care" for rural veterans with HIV. The rural primary care teams focus on reducing cardiovascular risk by treating high blood pressure, diabetes, high cholesterol, and tobacco smoking; checking bone density and renal function; and ensuring immunizations are up to date.
Results
Researchers offered the telehealth option to veterans who live closer to a CBOC or primary care clinic than to a VA hospital with HIV specialty care and who have to drive at least 90 minutes to one of these clinics. Most veterans (90% in the pilot studies) chose the telehealth option and were satisfied or very satisfied with their care.
Rates of HIV viral control remained high (over 90%) and smoking cessation care processes improved. Results for impacts on care outcomes in replication studies show improvement in retention in care in telehealth intervention clinics.
The HIV TCC program builds solid infrastructure foundations within participating VAs to integrate HIV specialty care to corresponding primary care Patient Aligned Care Teams with enhanced case management for rural veterans.
With the COVID-19 pandemic, there has been successful uptake of VA video connect visits, which has accelerated the uptake of telehealth technologies for HIV care in addition to enhancing the collaborative model between primary care and HIV specialists.
For more information about HIV TCC:
Ohl, M.E., Richardson, K., Rodriguez-Barradas, M.C., Bedimo, R., Marconi, V., Morano, J.P., … & Vaughan-Sarrazin, M. (2019). Impact of Availability of Telehealth Programs on Documented HIV Viral Suppression: A Cluster-Randomized Program Evaluation in the Veterans Health Administration. Open Forum Infectious Diseases, 6(6).
Further findings of the project are forthcoming.
Challenges
Rural primary care teams have multiple competing demands for their limited time. This barrier can be overcome by providing additional support to rural primary care teams with HIV care managers at the telehealth hub site who can work directly with veterans by telephone. This program uses primarily clinical video telehealth services but is also utilizing VA video connect and video on demand services to expand reach to rural veterans due to high demand.
Other barriers to care in rural areas are limited internet or cellular capabilities, despite the availability of specialists on these modalities. This program works with each participating site to work through options for connected care utilizing resource-specific amenities.
Replication
This program can be replicated in rural areas served by clinics with potential telehealth connections to HIV specialty clinics. Shared care relationships between distant HIV specialists and local primary care teams can start with a narrow focus on engaging primary care teams in cardiovascular risk factor management and can expand from there.
Some rural patients with HIV may prefer to attend telehealth visits in a clinic that is near enough to be accessible but far enough from home to avoid concerns about loss of privacy.
For other details on replication or interest in participating in this program from your affiliated VA, please contact the program lead listed below.
Contact Information
Jamie P. Morano, MD, MPH, Project LeadHIV Telehealth Collaborative Care Program
Jamie.Morano@va.gov
Topics
HIV and AIDS
· Telehealth
· Veterans
States served
National/Multi-State
Date added
July 21, 2017
Suggested citation: Rural Health Information Hub, 2024 . HIV Telehealth Collaborative Care (HIV TCC) Program [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/963 [Accessed 4 March 2026]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.