NC-REACH: NC-Rurally Engaging and Assisting Clients who are HIV positive and Homeless
- Need: Provision of medical care access and follow-up for rural North Carolina HIV patients with mental health, substance abuse, and unstable housing/homelessness challenges.
- Intervention: Medical home staff model expanded to a care coordination program with a core Network Navigator and Continuum of Care Coordinator assisting with medical, behavioral health, and basic life needs.
- Results: To date, the program has advanced three aspects of medical home patient care for this target population: provided further understanding of the spectrum of homelessness, including "hidden" homelessness; implemented outreach with creation of new community partnerships and a community housing coalition; and integrated medical care and behavioral health care for HIV.
Evidence-level
Effective (About evidence-level criteria)Description
 North Carolina has
high rates of HIV and high rates of newly diagnosed
patients. These patients usually have life challenges in
addition to their infection, such as medical and mental
health comorbidities. Other challenges associated with
the social determinants of health, like housing stability
issues, also impact these patients' lives.
North Carolina has
high rates of HIV and high rates of newly diagnosed
patients. These patients usually have life challenges in
addition to their infection, such as medical and mental
health comorbidities. Other challenges associated with
the social determinants of health, like housing stability
issues, also impact these patients' lives.
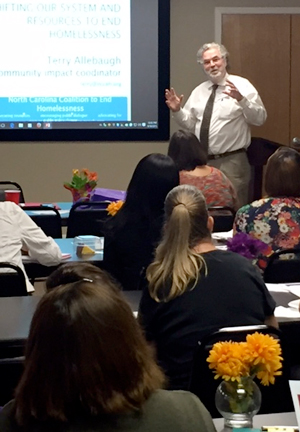
CommWell Health (CWH) is a Federally Qualified Health Center (FQHC) in Dunn, North Carolina. The organization offers integrated team-based medical, dental, and behavioral health services, with annual service numbers that have grown from 22,000 to 27,000 patients in a six county area in 2019-2020. For people living with HIV and AIDS (PLWH), CWH's Positive Life program also offers specialized comprehensive care for those patients living with the "triple stigma:" housing stability issues, mental health disorders and substance abuse.
 To further meet the needs of
these patients, CWH expanded its outreach by
participating in a Health Resources & Services
Administration's (HRSA) HIV/AIDS Bureau's national
initiative, an initiative that is part of the Bureau's
Special Projects of National Significance (SPNS). As the
only rural member of nine demonstration sites, CWH is
expanding both outreach and care.
To further meet the needs of
these patients, CWH expanded its outreach by
participating in a Health Resources & Services
Administration's (HRSA) HIV/AIDS Bureau's national
initiative, an initiative that is part of the Bureau's
Special Projects of National Significance (SPNS). As the
only rural member of nine demonstration sites, CWH is
expanding both outreach and care.
Several specific SPNS project strategies are geared towards meeting the following goals: improving timely diagnosis and initiation of HIV treatment; improving patient engagement and retention; assuring quality HIV primary care; and providing support services for individuals also experiencing homelessness or unstable housing. Additionally, specific attention is devoted to managing the co-occurring behavioral health issues and/or substance abuse disorders. As a result of these interventions, secondary goals emerge. These include increasing self-sufficiency and safety, sustaining sobriety, and fostering housing stability allowing a transition to the Positive Life program.
To implement these SPNS strategies and accomplish these goals, the unique skill sets of Network Navigators and Continuum of Care Coordinators are combined with services and skill sets of the internal and external CWH stakeholders.
Awards:
- North Carolina Community Health Center Association's 2017 Schmidt Outstanding Service Award
- National Rural Health Association's 2017 Outstanding Rural Health Program

Services offered
-
 Daily
huddles with SPNS team, Positive Life team, and CWH
behavioral health team
Daily
huddles with SPNS team, Positive Life team, and CWH
behavioral health team
- Provision of individualized client service plan, updated every 4 to 6 months
- Partnerships with internal stakeholders
- Providers with CWH's Behavioral Health Department
- Formal and informal partnerships with external stakeholders, such as community agencies and housing partners
- Regularly scheduled external stakeholder collaborative meetings
- Community outreach through community events
- Community educational outreach
- Health fairs, migrant farm festivals, churches
- Coordination with the Positive Life program
- Coordinated client service/progress documentation
Key team members on the specialized medical home comprehensive care team are:
Network Navigator
- Supports the HIV care team, providing intensive support to reduce barriers to care and foster continued connection to services
- "Voice of the Client" at comprehensive care team meetings
- Works within the community using a flexible schedule to assist with overcoming rural transportation barriers in order to meet appointment needs and health, housing, and supportive services
- Assists clients with obtaining needed public assistance, Medicaid/Medicare/ACA/Social Security enrollment, food stamps, housing, and other benefit programs services for basic needs: financial, medical, behavioral health, and housing
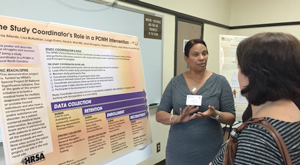
Continuum of Care Coordinator

- Experienced registered nurse specializing in infectious disease
- Coordinates with infectious disease physician to develop treatment program
- Provides individual clients with self-management education
- Works closely with network navigators to define additional client needs and solutions
- Performs client and program-related record keeping functions
- Comprehensive surveillance of the AIDS epidemic
Results
-
 Revealed "hidden
homelessness" (or "couch surfing" that is, moving
consistently between friends' and family's homes)
rates, rates not captured by state housing stability
data
Revealed "hidden
homelessness" (or "couch surfing" that is, moving
consistently between friends' and family's homes)
rates, rates not captured by state housing stability
data
- Emergence of "the ride that binds:" Client/navigator relationship development as a result of transportation assistance
- Some elimination of duplicative services within social service system
- Improved coordinated efforts with internal stakeholders
- All 80 NC-REACH clients attended at least one behavioral health assessment appointment
- 80 clients reached during the 12-month program
- 83% retention rate
- 75% of these clients demonstrated viral suppression as measured by lab results 12 months post-intervention
- Reduced stigma due to educational community outreach efforts
- Improved family relationships
Hear more about the program and its results in this video:
For more on this program:
Gomih, A., Banks, B., McKeithan, L., & Rajabiun, S. (2018). NC-REACH: A Rural Patient-Centered Medical Home for People Living with HIV Who Experience Unstable Housing. American Journal of Public Health, 108(S7), S525–S527.Challenges

- Recruiting housing partners with availability/readiness for program participation
- Staff recruitment and retention
- Internal and external expectation management
- Availability of safe, adequate housing for people who did not want to be in shelters
- Poor credit or incarceration history impact on housing applications
- Employment or financial assistance to maintain housing stability
Replication
 Future forms and tools
created by the NC-REACH program will include:
Future forms and tools
created by the NC-REACH program will include:
Setting up the Medical Home Model
- NC-REACH flow chart: follows client experience through the NC-REACH program from pre-intervention through transition of care
Enrollment and Contact Forms
- SPNS eligibility screening form: Assists with SPNS program eligibility determination
- Out of care outreach log sheet: Network navigators form for tracking client contact
- Stability acuity scale: Tool for assessing client mental health needs, substance use, housing needs, level of self-sufficiency, social support, domestic violence, and health status.
- SPNS contact form: Client's permission and best contact information
- Patient referral to NC-REACH form: External stakeholder referral form to the NC-REACH program
Contact Information
Lisa McKeithan, MS, CRC, Director of Positive Life and NC- REACH910.567.6194
LMcKeithan@commwellhealth.org
Topics
Behavioral health
HIV and AIDS
Home and community-based services
Housing and homelessness
Medical homes
The South
States served
North Carolina
Date added
October 2, 2017
Date updated or reviewed
November 30, 2020
Suggested citation: Rural Health Information Hub, 2020. NC-REACH: NC-Rurally Engaging and Assisting Clients who are HIV positive and Homeless [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/979 [Accessed 26 April 2024]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
