Aug 22, 2018
USDA Road Trip Through Rural America: Q&A with Anne Hazlett
 In June 2017,
U.S. Secretary of Agriculture Sonny Perdue named Anne
Hazlett as Assistant to the Secretary for Rural
Development. In that role, Hazlett oversees the USDA
Rural Utilities Service, the Rural Business Service, and
the Rural Housing Service and reports directly to
Secretary Perdue.
In June 2017,
U.S. Secretary of Agriculture Sonny Perdue named Anne
Hazlett as Assistant to the Secretary for Rural
Development. In that role, Hazlett oversees the USDA
Rural Utilities Service, the Rural Business Service, and
the Rural Housing Service and reports directly to
Secretary Perdue.
With prior leadership as the Chief Counsel to the Majority on the U.S. Senate Committee on Agriculture, Nutrition, and Forestry, Hazlett's duties include a key role in the Interagency Task Force on Agriculture and Rural Prosperity, the RD Innovation Center, and their opioid initiatives.
From Indiana, Hazlett grew up in a family of medical providers and gained an inside understanding of healthcare issues, especially those related to the social determinants of health. She graduated from Kansas State University with a Bachelor of Science degree in agricultural communications, has a law degree from Indiana University, and a master's degree in agricultural law from the University of Arkansas. Prior to public service, she practiced law with a focus on agriculture and environmental regulations. She was active in her home state of Indiana's agricultural issues as the state's Director of Agriculture and also served as a gubernatorial advisor and helped create Indiana's first Office of Community and Rural Affairs.
Rural healthcare providers and organizations might understand USDA as primarily associated with agriculture and Rural Development primarily associated with economic development. How can they best understand your agency?
We see our role as being a partner to local leaders, including rural healthcare providers, to build strong and healthy communities.
We see our role as being a partner to local leaders, including rural healthcare providers, to build strong and healthy communities. Rural Development's core mission is to increase rural prosperity.
To accomplish that mission, we focus on improving the quality of life and fostering economic opportunity through infrastructure, partnerships, and innovation with resources for utilities, telecommunication, housing, community facilities, and business development.
Though we have many tools available, to better understand our agency, I'd like to make several more points. Beyond tools, we have a tremendous resource in our staff. Unlike many other federal agencies, we have staff in every state — people who live and work in rural America. That presence allows our team to not only understand what's going on in the rural area that they serve, but also allows us to partner closely with local leaders. Additionally, our agency understands that no two communities are the same and that the best solutions really lie at that local level.
Noting the 4th of USDA's 7 strategic goals, "facilitate rural prosperity and economic development," where do you see rural healthcare playing a role in meeting that goal?
Really in a number of ways. First, rural healthcare systems keep people healthy so they can realize their fullest potential, whether that individual is starting a new business on Main Street or completing an advanced education degree that raises the income for a growing family. In addition to individual impact, rural healthcare systems are a significant source of economic activity in many rural places. I've seen some statistics that healthcare in rural areas can represent at least 20 percent of a community's employment and income, so they are real economic drivers in many towns.
Beyond the economic impact, I've seen that rural healthcare facilities often become a community center where a family's needs can be met. In my home state there's a town, Rushville, Indiana, where the local workforce development agency opened an office in an empty wing of the county hospital. Because the county hospital was a known locality, the community felt comfortable going there and getting assistance to better themselves.
With oversight of the Rural Utilities Service, the Rural Business Service, and the Rural Housing Service, how do you see these services intersecting with the social determinants of health?
The impact of that practice of medicine I watched growing up allows me to understand how the conditions in which people in rural America live influence their health.
I grew up in a medical family. My grandfather was an OB-GYN in a small town in western Pennsylvania. My father followed in his footsteps and just retired from a long and rather intense career of practicing cardiology. My mom is a nurse who cared for students at the local high school for years, a job that is more than just a student's healthcare needs. The impact of that practice of medicine I watched growing up allows me to understand how the conditions in which people in rural America live influence their health. USDA Rural Development resources include three buckets of tools — tools that help create social, economic, and a physical environment that can help promote good health for every American, no matter what zip code they live in.
I've seen specific examples of how USDA Rural Development activities are addressing social determinants of health during my recent visit to California, visiting the towns of Pixley and Poplar, two rural communities in the Central Valley. There we've recently invested $5 million in water infrastructure. This funding helped construct several new wells to provide safe drinking water for current residents — and future residents as these communities grow. With those wells also comes expanded opportunity for new business. That economic opportunity, in turn, can then create jobs and income for local families, thereby increasing the likelihood that the children in these families will grow up healthy.
The USDA is leading the efforts of the Interagency Task Force on Agriculture and Rural Prosperity. Tell us about the work the task force has already done and is planning for the future that might impact the health and well-being of rural residents.
Under Secretary Perdue's leadership, the task force issued a series of recommendations earlier this year. We're now moving forward with implementation of those recommendations. We've had several early successes. First, in the area of economic activity or broadband access, we're partnering with other federal agencies, White House leaders, the FCC, and the Department of Commerce to reduce regulatory burdens in order to develop infrastructure. In addition to the action on streamlining some of the federal permitting processes, we're also working to identify practices that can leverage federal assets for broadband deployment. Now we're moving forward with a new broadband pilot working with other agencies to reach rural communities about this opportunity.
Mapping is an issue we often hear about. In rural areas, who has broadband access, how do you know what's sufficient access, where is sufficient access located?
We know with these new resources we also have new opportunities to partner with agencies in policy, in funding, in outreach, and, importantly, in mapping. Mapping is an issue we often hear about. In rural areas, who has broadband access, how do you know what's sufficient access, where is sufficient access located? Mapping, then, is an important issue.
In another area of the report, quality of life, there was a recommendation to create greater access to modern healthcare services with specific reference to helping rural communities respond to the opioid epidemic. We're working directly with some other federal agencies, HHS and the Department of Justice, to see how we can layer our resources with theirs in order to have a bigger collective impact in rural areas.
I think all of this work will impact the health and the well-being of rural residents both directly and indirectly. Obviously, in quality of life, actions like increasing access to modern healthcare will have immediate measurable impact, but I think that there are more indirect actions that will have significant impact on quality of life and economic well-being for a rural resident — things like infrastructure and access to capital. We know our core mission is rural prosperity and, as opportunity grows through prosperity, we know the social determinants of health will also be impacted.
You have held a series of rural roundtables around the country looking at opioid misuse. What are the takeaways?
My own roots in the opioid crisis stem back to 2015. My home state of Indiana made national headlines when a small rural community, the town of Austin, Indiana, experienced an HIV outbreak of historic proportions, all due to injection drug use. I think watching the leaders of that small town fight on the frontlines of that battle had an enormous impact on me, initially because I saw the monumental toll that this issue can take on a rural community. The story of Austin, and the victory I've seen slowly emerging from that fight, has been a source of inspiration for me.
When we look at the quality of life and the economic opportunity in small towns, we simply can't talk about building strong and healthy communities without tackling the opioid crisis.
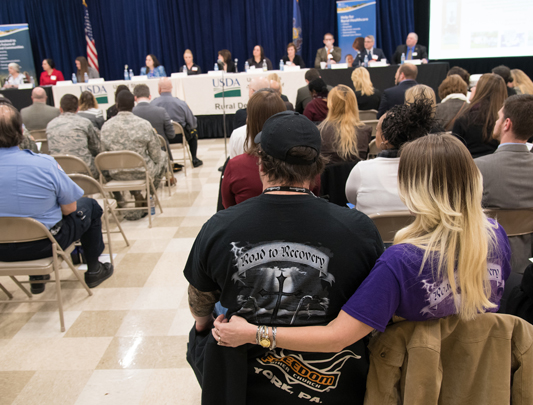
Now I've seen many other rural communities at these same crossroads. When we look at the quality of life and the economic opportunity in small towns, we simply can't talk about building strong and healthy communities without tackling the opioid crisis. This issue has been a top priority for this administration and there is an "all hands on deck" effort to fight this epidemic. The USDA's role in this again aligns with our core mission to increase rural prosperity. We've held roundtables in seven states (Pennsylvania, Nevada, Utah, Kentucky, Oklahoma, Missouri, and Maine) along with many less formal visits with numerous families and community leaders. Through those conversations we've gained a better understanding of the unique needs of rural communities and we've learned key lessons from what is already working on the ground.
One key lesson is that an effective response in rural America takes creativity in harnessing existing community assets, and limited resources mean we have to get creative. For example, in the context of prevention, we can't always just turn to school districts or sheriff's deputies who already have strapped resources and are stretched thin. What are the assets in a community that can be used as a platform for prevention? It's the "who": those who are already touching the lives of people living and working in rural America. When we take that creative lens, the sky is the limit in these rural areas. There are opportunities in churches, in the Cooperative Extension, in the Rotary, in the Lions Club.
I saw a real-world example of this lesson in Crawford County, which is a rural county in western Pennsylvania, with the Meadville Medical Center, a county hospital with a community foundation. They have taken the lead with creating a community conversation called the "Let's Talk" campaign focused on the disease of addiction. They have a website, they have community events featuring community members who give testimonials — all this helping the community recognize that addiction can happen to anyone.
While rural communities may lack resources because of their size, 'size' in rural is not something negative; it's something positive and a strength because of how quickly the messenger and an activity can make a difference.
A second lesson is how a small action step has a really big impact in rural America. A small step forward in a rural setting can have an enormous impact because it can quickly go viral in a way that couldn't happen in a large city. While rural communities may lack resources because of their size, "size" in rural is not something negative; it's something positive and a strength because of how quickly the messenger and an activity can make a difference.
A real-world example of this lesson is on the eastern shore of Maryland, Talbot County, with their campaign, "Talbot Goes Purple." Using a partnership between the local Rotary Club, the Sheriff, the county school system and the local community foundation, they've launched a community campaign using the color purple to help support families that are impacted by substance issues. They've got everything from shirts to towels at sporting events to actually changing out the Main Street lights to purple. Local leaders are literally painting the town purple to drive a community conversation about the dangers of opioids and other substances. I think when you're having that community conversation, you're reducing stigma and people are able to share their story and go and get help. That effort has actually been so successful that there are other counties in neighboring states that are looking to replicate it.
Though I have many other examples to share, here's a final lesson. In many rural communities, an effective response will include resilience that is built only through prosperity. This rural epidemic has been fueled by hopelessness and despair, stemming through lack of economic opportunity, feelings of isolation, and so to remedy that we can't just look at prevention, treatment, and recovery. Rural leaders really need to double down on addressing some of these deeper, systemic issues in rural communities — things like lack of broadband and the need to improve the quality of life, develop the next generation of the workforce, drive innovation, and increase economic development. When the upstream conditions in rural communities improve, there's a protective resiliency that builds that can prevent drug addiction really taking hold in the future.
What's going to come out on the other side of this crisis is a bright vision for the future. I find great hope in that.
Of examples around the country, I go back to the roots of my interest, my home state's experience with opioid misuse. In Scott County, Indiana, there is a "Get Healthy, Scott County" coalition that has become a catalyst for action going far beyond drugs. A group of local leaders meets every month and has difficult conversations around community issues: for example, transportation — a big challenge there — adult education, literacy rates, and parenting skills. These are hard conversations to have, but the leadership there is transforming that community. What's going to come out on the other side of this crisis is a bright vision for the future. I find great hope in that.
You've shared the importance of the USDA's Distance Learning and Telemedicine Program grants and website Opioid Misuse in Rural America. Both of these opportunities lend to another rural healthcare challenge: rural broadband connectivity. What do you see as the most important next step in meeting this healthcare connectivity challenge?
The most important next step in meeting the connectivity challenge is innovation in how we deliver that connectivity. We have a unique opportunity right now to innovate with some new resources that were given to us by Congress through a $600 million broadband pilot program. Let me state the obvious: It's exciting because that's a significant increase in our available resources. But, it's even more than that. In addition to resources, the pilot program gives us some flexibility in our authority and, with that, we have a unique opportunity to innovate in our funding delivery structure as well as who can participate in the program. For example, are there new opportunities for an electric cooperative who's already serving a rural community to partner with an existing community-based telecom to provide broadband to that community? This is a new program with a responsibility we're taking very seriously as funding stewards designing a program to have the biggest impact. We've opened up a public comment period that runs through early September that will allow us to gather some stakeholder feedback on the parameters of this program.
When I think about specialized medical care or treatment needs for the opioid crisis, we know that there are critical healthcare needs that need to be addressed through broadband connections. We would welcome the input of rural healthcare providers into this process.
When I think about specialized medical care or treatment needs for the opioid crisis, we know that there are critical healthcare needs that need to be addressed through broadband connections. We would welcome the input of rural healthcare providers into this process.
Opinions expressed are those of the interviewee and do not necessarily reflect the views of the Rural Health Information Hub.

