Nov 27, 2024
Building a Rural Cancer Care Network: Federal Funding Supports Collaboration of Urban, Regional, and Local Organizations
What do an urban nonprofit organization, a regional healthcare system with rural locations, and a local rural physician's office have in common? Collaboration with a shared goal to create the Southeastern Rural Cancer Care Network to bring rural Georgians access to comprehensive cancer care.

The Southeastern Rural Cancer Care Network partners are leveraging a Federal Office of Rural Health Policy Rural Health Care Coordination Program grant to create the network. Cheryl Kirby is the network director for the grant's lead organization, Georgia CORE (Center for Oncology Research and Education), a nonprofit organization with a goal of reducing the burden of cancer in Georgia through research, education, and advocacy.
"Georgia CORE recognized the unmet needs of cancer patients in the rural areas of southeastern Georgia," Kirby said. "Based on its long-time relationship with the Nancy N. and J.C. Lewis Cancer & Research Pavilion (LCRP) at the St. Joseph's/Candler Health System in Savannah, Georgia, Georgia CORE reached out to them as a network partner for this project."

Ashley Gravely, RN, is the project's regional oncology patient navigator (ROPN). As part of LCRP in Savannah, Gravely lives and works at one of the grant's rural locations in Jesup. She summarized the grant's activities.
"I can't say it better than an explanation I heard given by someone else: We are bringing big-city resources and care to little-city places by meeting the patient where they are," she said.

Nursing administrator Bobbie Jean Curkovic, DNP, director
of Infusion and Supportive Services at the LCRP, weighed
in.
"Caring for cancer patients is holistic patient care," she said. "It's addressing barriers to care and helping patients navigate through the complexities of a healthcare system. Along with much, much more, this framework is what this project is about.
"We also have the responsibility to be the voice of the rural customer that not only needs infusion services, but other cancer treatments, like radiation. By using care coordination and transition care management models, we are addressing the social determinants of health that have proven links to optimal patient health and well-being."
Southeastern Rural Cancer Care Network
Grant Collaborative Partners
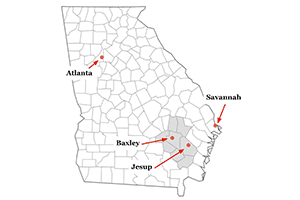
- Georgia CORE Center for Oncology Research and Education, Atlanta
- Joseph's/Candler Lewis Cancer & Research Pavilion, Savannah
- Appling Healthcare, Baxley
- Wayne Memorial Hospital, Jesup
- Jeyanthi Ramanarayanan, MD, St. Joseph's/Candler hematologist/oncologist with offices in Baxley and Jesup

Common Experiences Yield Early Results
Acknowledging that grant-supported work that involves urban and rural partners might seem to potentially complicate collaborative project work, Gravely, Curkovic, and Kirby shared that their work feels seamless and collaboration is easy — which definitely has influenced the success of their deliverables and benchmarks during their planning year.
The three project members attribute this success to a common theme.
"We've all had personal lived experiences connected to the rural cancer patient," Curkovic said. "We understand, and that intimate level of familiarity with rural cancer patients' needs brings a unique understanding to the collaborative troubleshooting and problem-solving challenges around the grant goals."
Kirby elaborated.
"The project title is a snapshot of our work: Achieving adequate healthcare access for rural cancer patients through navigation linked to care coordination leads to increased access to care," she said. "Another part of the project's big picture is gaining access to clinical trials."

Preventing the "This Is Just Too Much": Understanding Rural Oncology Patient Navigation
"Our work started with exploring the best approaches to reducing barriers to care and that's where the oncology patient navigator comes in," Curkovic said.
From her perspective as a nurse and nursing administrator, Curkovic said she's noted a specific element linked to the patient navigator role in this project's work: Although it is oncology-specific, it is also rural-specific oncology patient navigation, different because it's happening in low-resource environments.
We believe that what we're discovering about rural oncology patient navigation will add to the elements of traditionally urban-informed models.
"With the grant funding part of Ashley's role, we're seeing how navigation clearly helps efforts so that cancer care becomes more than just the medicine but becomes whole-person care, especially when the social determinants of health are attended to," she said. "Ashley is our most rural navigator. Despite the low-resource environment, she's finding creative ways to address the unique rural social determinants that cause barriers to cancer care. Even this early in our project, it's difficult to contain our enthusiasm for what she's accomplishing as she encounters so many unanticipated challenges. We believe that what we're discovering about rural oncology patient navigation will add to the elements of traditionally urban-informed models."
Gravely reviewed some of her non-clinical activities, sharing that much of their population is low-income with financial barriers to many resources that are often taken for granted. There are not just struggles with food security, but also adequate clothing. Transportation, in particular, stands out as a challenge looming even larger as a more urgent barrier because getting cancer treatment often depends on travel. One solution has been creating a process to provide gas cards to assist patient transportation needs.
Gravely said there is another equally important social need: someone to trust in times of emotional vulnerability.
"I put myself in the patient's shoes," she said. "With a cancer diagnosis, I'm going to be terrified. I'm going to want somebody I can trust. So, I tell patients, 'I'm that somebody. I'd like you to trust me.'
"I also tell patients that my phone is just for calls from them. It's so important that they don't feel alone. If they feel like they're overwhelmed by the questions in their head like, 'Who am I supposed to talk to next? What am I supposed to be doing?' I tell them that's what I can help with."
Moving to the clinical aspects of her work, Gravely pointed to care coordination, a focus of the grant-funded project. For example, she said that coordinating patient care also includes coordinating multiple appointments that are not always in the same health system. This coordination is vital to ensure that patients have access to the care they need — especially knowing that research proves that this type of patient care coordination not only impacts treatment adherence but impacts survival outcomes.
She said she recognizes that her perspective as a clinician is a perspective completely foreign to patients, necessitating that she attends to the specifics of care coordination with careful explanations of what should happen during appointments and details about treatments ordered. Although cancer care usually follows a logical sequence, she said it's also not unusual for the sequence to be disrupted by unique or unforeseen circumstances, perhaps more common in low-resource rural areas.
Gravely said she's gaining more knowledge about how to "navigate" these situations.
"Rural cancer care is unique and complex," she said. "These patients benefit from a go-to person like an oncology patient navigator to help them get on and stay on the right path," she said. "If that assistance isn't there, patients will just say, 'This is just too much. I can't do all this.'"
Leveraging Grant Funding Support
In addition to partial support of the ROPN role, project leaders explained the value of grant support for site meeting attendance and networking at other in-person events throughout the state, value that's also evidence-informed.
"Although virtual meetings have great value, in-person meetings where we can talk frankly with others from across the state involved in this project is so important to our work," Kirby said. "It's also the environment where we not only learn from each other, but where others become aware of the network we're building. Meetings are also where we have the privilege of sharing our early accomplishments so others might begin to duplicate or build on our successes and begin using the network."
Curkovic and Kirby also talked about other project details, including their use of evidence-based tools around oncology nurse navigation, chronic condition care coordination and transitional care (TCM) services, in addition to region-specific and local tools, including their own resource mapping.
"When a project of this scope starts, one of the first actions is to complete an asset mapping and gap analysis," Curkovic said. "This work was one of the most rewarding endeavors of my career. All that effort produces an early and vital resource for the grant's activities."
From the Physician's Perspective: More than Just Increased Cancer Care Access

Jeyanthi Ramanarayanan, MD, a specialist in hematology and oncology, is another clinical partner in the project. She, too, said it's hard not to be impressed with collaboration's early impact on cancer care access for the rural people she serves in Jesup and Baxley.
"This past year-plus has brought rapid changes," she said. "We went from a part-time oncologist to my being able to provide full-time hematology and oncology services. The clinic got set up, referral processes were put in place, along with triaging algorithms — overall a major expansion in services."
However, she pointed out it's one thing to have services in place and another to have patients know about them and take advantage of them.
Ashley's a trusted member of this community and I think we're seeing a major word-of-mouth impact.
"Offering both hematology and oncology services was important and with the grant in place, our volume has already increased about 50% in the past year," Ramanarayanan said. "I have to tell you, this sudden increase has been a big surprise. Ashley's been getting the word out, along with some of the hospital marketing teams. Ashley's a trusted member of this community and I think we're seeing a major word-of-mouth impact. We're growing and with growth comes expansion of additional services."
In particular, Ramanarayanan said she believes — linked to the collaborative network-building and care coordination — this expansion has had an impact on increasing surgical care in this rural area.
"We've now got new surgeons at Wayne Memorial," she said. "We had one surgeon and now we have three. This means colon cancer, breast cancer, and other cancer surgeries can be done here locally. If the surgery is more complicated, they have privileges at the more urban hospitals. They can do the surgery there, but follow-up can be done locally. We also know that with our grant focus on care coordination and a multidisciplinary approach to build a network infrastructure, this location becomes attractive to new physicians. We can be hopeful about expanding services even further and potentially be able to bring in other specialty care, like a pulmonologist and gastroenterologist, in the future."
Not To Be Overlooked: Increasing Rural Patients' Access to Cancer Clinical Trials
As defined by the U.S. Food and Drug Administration, clinical trials are "research studies in which people volunteer to help find answers to specific health questions. When carefully conducted, they are the safest and fastest way to find new treatments and ways to improve health." (definition no longer available online)
A recent academic article provided this rural perspective around the benefits of clinical trial participation for rural populations:
"…Clinical trial participation is a strong and consistent predictor of more positive cancer outcomes, and when considering only those who were enrolled in clinical trials, rural and urban residents experienced similar cancer outcomes."
The authors continued, acknowledging barriers and solutions to remedy the fact that "clinical trial accessibility for rural patients continues to be low."
Back to Kirby's project snapshot, Kirby and the other team colleagues in Atlanta, Savannah, Jesup, and Baxley said they are adamant about achieving the project's goal of increasing rural patients' access to clinical trials. Kirby pointed to Georgia CORE's relationship with those providing clinical trials at Atlanta's Georgia National Cancer Institute Community Oncology Research Program, Northside Hospital Cancer Institute, and the clinical trials available at Savannah's LCRP. Connecting with these established networks is part of the grant's work.

Noting that Gravely currently screens all new patients for potential clinical trial enrollment, Ramanarayanan added that with the efforts of building this network and establishing relationships with organizations doing clinical trials, when referrals are needed, they've now been expeditious. However, she pointed out that the "financial toxicity" associated with cancer care is always a consideration around trials — especially for rural Georgians in her service area — because travel is usually involved.
With her early career including an American Society of Clinical Oncology Young Investigator award and research experience at Roswell Park Comprehensive Cancer Center, Ramanarayanan said she looks forward to the possibility of being involved with local clinical trials. In addition, she'd also like to do rural-based research to build understanding and bridge the rural gaps to these options.
Yet becoming a clinical trial site is a separate journey. Curkovic pointed out that the first step is accomplished by offering hematology/oncology care locally. The next step is to gather information about the community's interest in participating if there were clinical trial options.
"We're not a designated clinical trial site," Curkovic said. "That takes about a year. Right now, I've just submitted the IRB [Institutional Review Board] request to gain permission for Dr. Ramanarayanan to survey patients in her own practice around their perception of clinical trials to help us create a foundation for offering these."
Addressing Sustainability
Knowing grant support eventually ends, Kirby said sustainability looks very promising. With patients able to access local care, care coordination in place, networks established, and supports in place so low-resource patients can overcome the SDOH barriers they're experiencing, the elements needed for sustainability are in place.
Expected Project Outcomes
Short-term:
- Provide patient navigation services
- Introduce coordinated care to reduce the time to treatment
- Create seamless transitions to tertiary cancer centers when necessary
- Address social determinants of health barriers to timely care
Intermediate:
- Increase access and enrollment to clinical trials
- Share knowledge around evidence-based practices specific to rural cancer care disparities in cancer
Long-term:
Improve survival by:
- Increasing early detection, intervention, and treatment
- Reducing comorbid condition-linked complications
- Decreasing cancer incidence rates through prevention, education, and improved timeliness to care
Source: Rural Health Care Coordination Program Directory, 2023-2027 (no longer available online)
Ramanarayanan pointed to another item on the list that she said she believes increases sustainability potential: community trust.
She also suggested another way this network has sustainability potential: Creating inspiration for future possibilities because this network is in place.
"We can be building evidence to inform federal and state policies around rural cancer care," she said, again mentioning specific rural needs like addressing cancer financial toxicity and the current early work on this issue with a college of pharmacy at one of Georgia's universities.
"We're doing things like exploring what we can offer as telehealth check-ins for patients after their first round of chemotherapy," she said. "Building on this network allows for participation in so much, like working with other cancer-centric committees, and to include even working with those focusing on treatment and resources for pediatric cancer care and telehealth for the more frail older cancer patients.
"All of this action is important because with networks in place, we can be the ones representing rural populations at these tables," she said.

