Mar 16, 2016
Counteracting the Darkness of Physician Burnout
by Jenn Lukens

It was 2008 when Dr. Jill Kruse, fresh out of residency, took a job at St. Michael's Hospital Avera in Tyndall, South Dakota. As a young primary care doctor, she was eager to put her years of school to use and took on anything that was asked of her. Within a few years, she became the medical director for the nursing home, the overseer of the town's emergency medical service, the football team's sideline doctor, the clinic's medical director, and the hospital's trauma director and chief of staff. Kruse also shared rotations and call with only one other physician and two physician assistants to serve a town of 1,200 people.
Four years later, the demands of rural practice, coupled with trying to raise a young family, had started to take its toll. Her husband was the first to notice that she was becoming burned out. "He urged me to get a different job, saying 'you are killing yourself slowly in front of my eyes, and I'm not going to watch it happen,'" recalls Kruse.
If I am going back, something has to change. I can't go back to the same way, or I won't survive.
She admits trying to hide the burnout behind a brave face while working even harder, but that strategy only made it worse. Kruse was at her limit and didn't know where to turn.
Then, her second child was born. During maternity leave, Kruse began questioning if she was even going to return to work. She remembers thinking, "If I am going back, something has to change. I can't go back to the same way, or I won't survive."
Burnout in Rural Settings

Randall Longenecker, MD, FAAFP, serves as assistant dean for rural and underserved programs at the Ohio University Heritage College of Osteopathic Medicine and is the Executive Director of the national RTT Collaborative. He is an advocate of teaching medical students and residents skills to build their resilience and help them deal with the stresses of rural practice.
Longenecker points out that the recent spotlight on physician burnout doesn't mean it is a new issue. "There is clearly more publicity, but physician burnout has been an ongoing problem in medicine, both rural and urban," observed Longenecker.
In Longenecker's experience, rural settings can actually encourage providers to admit they have a problem. "One of the advantages of living in a 'glass house' where everyone knows each other's business is that (burnout) quickly becomes apparent to others," said Longenecker. As in Kruse's case, it is often a third party who initially notices the burnout and encourages a change.
Providers who build strong relationships within their community also have an advantage when dealing with burnout. "Resilience, or the ability to persist and thrive through hardship, is a competency for a rural practice," commented Longenecker. "Hardship itself is not the most important contributing factor (to physician burnout), the lack of healthy relationships is."
The Downward Spiral
 While in Tyndall,
Kruse sought help from Dr. Dike Drummond, CEO of thehappymd.com,
physician coach and healthcare speaker, who specializes
in physician burnout. Through regular coaching sessions,
Drummond walked her through burnout coping strategies
that started a path toward healing.
While in Tyndall,
Kruse sought help from Dr. Dike Drummond, CEO of thehappymd.com,
physician coach and healthcare speaker, who specializes
in physician burnout. Through regular coaching sessions,
Drummond walked her through burnout coping strategies
that started a path toward healing.
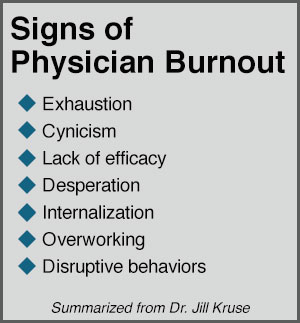
Drummond teaches that the difference between stress and burnout is the ability to recover in your time off. Physician burnout accelerates when there is no time set aside to recharge. This results in a downward spiral characterized by physical and emotional exhaustion, depersonalization with patients, and a reduced sense of personal accomplishment.
Kruse can attest to the necessity of recharging. Her lack of it made her feel like she was constantly withdrawing money from an overdrawn checking account. "You keep writing checks, but they continue to bounce, and there is no way to get back in the black," explained Kruse.
Making a Change
Slowly, Kruse started to see improvement, but not without a struggle. After exhausting all of Drummond's coping methods, she realized that the pressure of two children, multiple responsibilities at work, and a strict call schedule was simply unsustainable. "It became very evident that this was not the right clinical fit for me in this stage of my life," said Kruse.

In 2013, Kruse and her family moved to Brookings, South Dakota, a town of 22,000, where she started working at the Avera Medical Group Brookings. The change was exactly what Kruse needed. The increase in time allowed her more energy to put toward being a better mom and doctor, engaging with her patients the way she used to. "When you are not burned out, you can go the extra mile to talk with patients and meet their entire need. Now, I can enjoy the relationships that come with practicing medicine. I feel like I'm a healer, not just a physician," said Kruse.
Now, I can enjoy the relationships that come with practicing medicine. I feel like I'm a healer, not just a physician.
Eventually, she wanted to start sharing the burnout recovery methods she learned with her medical community. Kruse was hired as medical director of Avera LIGHT, a physician burnout prevention and coping program launched by Avera Health with a dedicated budget. The program was specifically designed for physicians, physician assistants, and nurse practitioners within Avera's healthcare system. A LIGHT steering committee composed of physicians, advanced practice providers, and administrative leaders provide oversight and strategic direction. Mary Wolf, Avera's Employee Assistance Program director, also serves as Avera LIGHT's program director.
Avera LIGHT
The name, Avera LIGHT, comes from the image that Kruse explained, "As opposed to a candle burning at both ends, we want our providers to be a light that counteracts the darkness of burnout." LIGHT is also an acronym for their program's goals: Live, Improve, Grow, Heal, and Treat.
 Through executive
coaching, accountability, and practical steps to improve
work-life balance, Avera LIGHT helps prevent burnout and
heal providers who have gone through it.
Through executive
coaching, accountability, and practical steps to improve
work-life balance, Avera LIGHT helps prevent burnout and
heal providers who have gone through it.
Because of the perceived stigma that often accompanies seeking mental or emotional help, most services like Avera LIGHT have difficulty getting people in the door. Kruse says that the first step is for a provider's attitude to change from feeling ashamed to admitting that they need help.
Even though burnout is very common, it's not normal and we rarely talk about it. We want our medical professionals to know that their work doesn't have to feel like this. We can make things better.
"Even though burnout is very common, it's not normal and we rarely talk about it. We want our medical professionals to know that their work doesn't have to feel like this. We can make things better," said Kruse. The fact that Avera LIGHT attendees and conversations are kept confidential has helped in convincing providers to come forward.
Since its launch in 2014, Avera LIGHT's services have had positive effects on Avera's staff. After going through the courses, physicians who have been on the brink of quitting their jobs have chosen to stay on staff. More providers are accessing employee assistance programs that were previously left untouched, and those who have benefited from the program are becoming peer coaches to help their fellow physicians. Kruse recalls one physician who approached her after a seminar. "He said he was so burned out that he saw suicide as the only option. After receiving the help he needed, this physician is already interested in helping others," relayed Kruse.
Building Resiliency
The efforts Avera LIGHT is making to minimize physician burnout are part of a national trend among healthcare and educational facilities. Medical schools like Sanford School of Medicine at the University of South Dakota are starting to adopt wellness programs and integrate physician burnout prevention into their curriculum. As a board member of the South Dakota State Physician Burnout Committee, Dr. Kruse has helped with this process.
Longenecker says that the number of physicians who quit due to burnout is hard to measure, since it often goes unrecognized or is attributed to other factors. He has seen many doctors leave their practice due to burnout, only to go on to other places ill-equipped to handle the conditions they will inevitably face again.
To prevent this, Longenecker says that resiliency, or "the capacity to endure and overcome hardship," needs to be a key competency for rural medical providers. This is not to be taken as an encouragement to endure harmful situations, but to understand personal and professional limits.
Those who are most susceptible to burnout in rural practice are those who fail to recognize and embrace their limits and work within them.
"Those like Dr. Kruse who acknowledge burnout and do something about it become resilient," assured Longenecker. "Living with scarcity and limits has been identified as a competency for rural practice. It refers not just to limited resources, but to maintaining healthy boundaries and guarding margin for self and family. Those who are most susceptible to burnout in rural practice are those who fail to recognize and embrace their limits and work within them."
In his journal article, "Teaching and Learning Resilience: Building Adaptive Capacity for Rural Practice," Longenecker and his co-authors outline these four main steps for building resiliency:
- Embrace hardship as an opportunity for growth
- View resilience as both an individual and community property
- Pursue adaptability more than hardiness
- Set a lifelong pattern of learning this competency in practice
From One Professional to Another
As an experienced doctor in a rural community, Kruse has a wealth of advice for rural medical administrators, starting with budgeting. "Make room to pay locum doctors to take weekend calls. You are going to lose your doctors if they are constantly working and never getting a chance to recharge," suggests Kruse.
She also recommends actively looking for burnout signs among providers and offering them support. "It can be very isolating in a rural community. Find ways that your doctors, especially new graduates, can connect with someone that understands. Be the mentor that helps them flourish as opposed to throwing them in the deep end and hoping they can swim."
Dr. Longenecker encourages administrators to look beyond productivity levels and the financial bottom line. "I believe it is as important to reward creativity, agency, community engagement, and relationships as it is to act with integrity and fiscal responsibility."
