Jun 01, 2022
RESEP Clinics Help Rural Residents Access Care and Compensation After Radiation Exposure
by Allee Mead
 The United States
government-led nuclear weapons testing from 1945 to 1962
and uranium mining from 1943 to 1971 exposed workers,
their families, and others living near the mines or
testing sites to harmful levels of radiation that can
lead to cancer and other illnesses.
The United States
government-led nuclear weapons testing from 1945 to 1962
and uranium mining from 1943 to 1971 exposed workers,
their families, and others living near the mines or
testing sites to harmful levels of radiation that can
lead to cancer and other illnesses.
 The
Radiation Exposure Screening and Education Program
(RESEP) was created in 2000 through amendments to the
Radiation
Exposure Compensation Act (RECA), which provides
compensation to individuals who were exposed to radiation
from the mining or nuclear fallout and subsequently
developed certain health conditions. RESEP grants are
awarded to healthcare organizations so they can provide
screenings, referrals for medical treatment, assistance
with RECA applications, and education and outreach.
The
Radiation Exposure Screening and Education Program
(RESEP) was created in 2000 through amendments to the
Radiation
Exposure Compensation Act (RECA), which provides
compensation to individuals who were exposed to radiation
from the mining or nuclear fallout and subsequently
developed certain health conditions. RESEP grants are
awarded to healthcare organizations so they can provide
screenings, referrals for medical treatment, assistance
with RECA applications, and education and outreach.
Grants are awarded through the Health Resources & Services Administration (HRSA). Healthcare organizations are eligible if they're located in one of the 12 states considered most affected by the testing and mining: Arizona, Colorado, Idaho, Nevada, New Mexico, North Dakota, Oregon, South Dakota, Texas, Utah, Washington, and Wyoming.
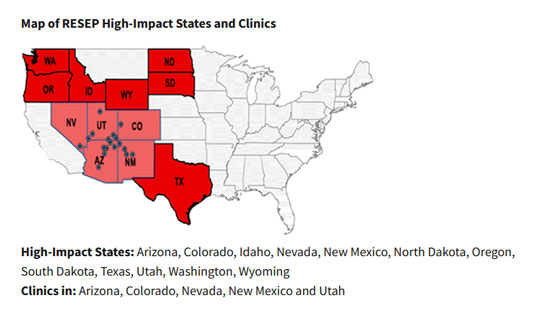
Current RESEP clinics are located in Arizona, Colorado, Nevada, New Mexico, and Utah. Two of the longest-standing grantees are the Navajo Area RESEP and the Southwestern Utah RESEP.
Jason Rush, the former RESEP Program Coordinator, reported that the Southwestern Utah team has a 94% "RECA claims awarded" rate from the Department of Justice, and he called Northern Navajo Medical Center (NNMC) "an integral resource to the Navajo community."
He continued: "Not only is Navajo Nation dealing with the impacts of historical uranium exposure, but also with persisting exposures due to abandoned mines on Navajo Nation that have not been entirely cleaned up. While they were active, these mines produced a great deal of environmental damage in the form of waste products leaking into communal water sources and uranium dust being dispersed throughout the soil in the process of transport. NNMC has done a great deal to offer services to individuals who fall into both historical and contemporary exposure categories."
"In the wrong place at the wrong time"
In the 1950s, there were discussions at the federal level about making sure the uranium mines were ventilated, but it was left up to the states and mine owners to take these safety measures. "I think the big picture of getting the uranium and the money for selling the uranium by the mine companies and mine owners really overshadowed what was best for the individual miners," Denise Bartley, project director of the Navajo Area RESEP program, said. "And nothing was really done until it was forced to be done."

That lack of safety measures as well as education about radiation affected not only the workers but also their families. Some patients at the Navajo Area RESEP program have shared stories of having a father who worked in one of the mines: how they'd run outside to give him a hug while he was still covered with dust from the mine and how they'd wash his work clothes in a rain barrel or nearby stream or hang them on a clothesline and beat the dust off them. "It's all this secondhand exposure that they were getting just by being helpful and doing their chores," Bartley said.
Bartley, a family nurse practitioner, has worked at the Northern Navajo Medical Center for over 20 years and has worked with RESEP and Community Uranium Exposure—Journey to Healing Program (CUE-JTH) for five years. Her uranium programs also work closely with the Navajo Nation Environmental Protection Agency to address issues of environmental injustice.
The United States Environmental Protection Agency (EPA) recognizes over 500 abandoned uranium mines on Navajo lands. "People didn't move to the uranium mine; the uranium mines went in right next to the people or the community," Bartley said. "It wasn't like they had a choice and then they ended up paying the price."
Rebecca Barlow, project director of the Southwestern Utah RESEP clinic and a family nurse practitioner, works primarily with downwinders, people who lived downwind from nuclear testing sites. "The people that lived here at the time of the nuclear testing were just unfortunate enough to be in the wrong place at the wrong time," Barlow said.
Services and success stories
The Southwestern Utah RESEP clinic, created in 2003, is part of Intermountain St. George Regional Hospital. Due to its location, the Southwestern Utah RESEP clinic's main patient population is downwinders who lived in certain counties in Arizona, Nevada, and Utah during the qualifying timeframes.
The Southwestern Utah RESEP clinic has two components: a cancer screening and education program and compensation assistance. In the first component, clinic staff complete a cancer screening physical; go over the patient's medical, work, and family history; and complete a risk assessment. In the second component, patients who have been diagnosed with one of the qualifying cancers or respiratory or kidney diseases get help applying for RECA compensation. Whether or not a patient qualifies for compensation, they are referred to Intermountain Healthcare providers to address their health conditions.
It is the goal of our RESEP program to continue to educate as many people in the exposed areas as possible about their increased cancer risk.
Barlow said that before the Southwestern Utah RESEP clinic was established, the service area did not have a clinic devoted to providing education about health issues related to nuclear fallout. As a result, many individuals did not have routine cancer screenings. Her clinic works to make sure patients better understand the reasoning behind screening recommendations. This education also extends to local primary care providers so they can better understand their patients' unique health challenges. "It is the goal of our RESEP program to continue to educate as many people in the exposed areas as possible about their increased cancer risk," she said.

The Southwestern Utah RESEP clinic has served over 5,600 patients since 2003 for potential cancers and other diseases related to radiation exposure. Over two-thirds of patients have been referred for further testing, either because an abnormality was found or because the patient was due for other preventive screenings like a mammography or colonoscopy.
The clinic has also given out general RECA information to over 103,000 people and distributed over 34,000 brochures and 3,800 RECA applications. The RECA counselor has completed over 60,000 RECA counseling sessions and has helped over 1,700 people get compensation (a total of over $85 million). This counselor is currently working with 200 active RECA claimants.
Barlow credits part of her clinic's success to the Intermountain Healthcare system, especially its "cohesiveness." She remembers a patient who she suspected had breast cancer; she was able to immediately connect the patient to another Intermountain Healthcare provider to start the work-up. Patients can access cancer screenings and work on RECA applications in the same building.
Barlow also credits HRSA, the Federal Office of Rural Health Policy, and the Department of Justice: "The project managers and claim examiners we have had over the years have been so supportive and consistently gone out of their way to help us be successful. They are always available to ask for advice and clarification, and if they don't know the answer, they will find someone who does."
Northern Navajo Medical Center, which houses the Navajo Area RESEP program, is a 60-bed hospital with a Level IV trauma center and a traditional healer. "It helps us bridge the gap between Western medicine and traditional medicine…so we can have the best health outcome that we can have, and that includes spiritual as well as physical," Bartley said.
Acknowledging distrust and listening to patients
Bartley said many of the uranium workers, their family members, and community members feel disrespected by the apparent lack of concern for their safety. "They had to take the majority of the risks," she said. This population, naturally, can be distrustful of federal agencies, including Bartley's work. "I know the anger and mistrust that the Navajo people feel is sometimes directed toward me, but it is not about me," she said. "I'm in a good position to take small steps to help with the healing process. And that's what I try to do. Every time I come into that situation, I remind myself that this past trauma is very real and is continuing to impact the person or family in front of me. I try to help with the healing by being transparent and acknowledging the past trauma that the person has encountered."
Every time I come into that situation, I remind myself that this past trauma is very real and is continuing to impact the person or family in front of me. I try to help with the healing by being transparent and acknowledging the past trauma that the person has encountered.
Bartley said that she builds a rapport with patients through being honest and listening to them: "Many times the person just wants to be heard. And I think that a lot of times we don't take the time to listen, or we think we already know what their history is…I can't go back and fix the problems brought about by uranium mining or people having secondary exposure because of it, but I can listen to and validate what they're saying and hopefully they feel better, like they feel that somebody's finally heard them as an individual."
Some children of uranium miners shared that they used to drink water from a stream that had filtered down to the uranium mines, since the water there was cold, or they would play around the mines. These patients often blame themselves, but Bartley tells them, "Of course you didn't know this was dangerous. Nobody told you. You were children." She added, "I hate when they feel responsible…Of course you didn't know. This is not your fault."
Bartley also knows clients with post-traumatic stress disorder (PTSD) symptoms from listening to the blasting in the mines and dealing with the subsequent dust storms.
Barlow from Southwestern Utah echoed Bartley's thoughts on their patients' distrust: "Many of these patients feel that, at the time of the nuclear testing, the government lied to them about the potential harm involved. This makes some of them not trust the recommendations made by today's government regarding the stated health risks and cancer screening recommendations."
A lot of what we do is just listening to them tell us about their experience with the bombs growing up and their experience to the exposure of sweeping the ash off their porches or playing in the ash in their gardens and different things that have happened since then.
Barlow also agreed that listening is a key component of her work: "A lot of what we do is just listening to them tell us about their experience with the bombs growing up and their experience to the exposure of sweeping the ash off their porches or playing in the ash in their gardens and different things that have happened since then."
Other challenges for patients and providers
Given the size of the service area — NNMC serves people from New Mexico, Arizona, and Utah — transportation is a huge challenge for patients seeking services. "There are over 18,000 miles of roads on the Navajo Nation," Bartley said, "and only about 3,000 of those miles are paved. Further, almost 33% of households do not own a vehicle and public transportation from a person's home is non-existent." In order to help the elders, who do not drive, the contact representative for RESEP will do some home visits to assist with RECA claims and the CUE-JTH staff holds community-based screening events.
Bartley said it's also important for providers to understand why patients may miss appointments: "The roads are bad. The weather may be bad. We've had horrible windstorms as of late…Some of our area on the Navajo Nation does not have cell phone coverage. People have cell phones, but they can't call out at certain times or from certain locations." She urged providers to be flexible if a patient shows up late or early to an appointment.
Transportation is a challenge for the Utah clinic as well. Barlow and her team serve an older population, some of whom live 150-190 miles away from the clinic in St. George. Some of the clinic's patients don't have insurance, so they may struggle to access cancer screenings. "It can be frustrating that while we educate our patients in what they need to do to protect themselves, if they are unable to get the tests done, we haven't accomplished what we need to," Barlow said. Barlow's team uses community outreach events to educate people about the program and different community resources.
Barlow said that there are misconceptions about who qualifies for RECA compensation: "Some people think that you have to be alive to apply and some people think you have to have died to apply. Many people don't understand that spouses, children, and grandchildren can apply if the claimant has passed away. Getting the information out to people is one of the most important things we can do." People who lived in the area at the time of testing but later moved away also qualify for services and compensation. Barlow's team has worked with some patients remotely.
Even though the compensation part is ending, you can't quit screening and really trying to improve health outcomes for this group of people.
Bartley from the Navajo Area RESEP said that, unless there is new legislation to renew it, RECA compensation will end in July 2022. But she and her team will continue to work with their service population: "Even though the compensation part is ending, you can't quit screening and really trying to improve health outcomes for this group of people."
Tools for success
Word of mouth, Barlow of Southwestern Utah said, is her clinic's most powerful tool for finding potential claimants. "At our clinic we recognize that for every person that we see, either in clinic or at outreach events, there is potentially an entire family or community of people that may also qualify," she said.
"The community itself was affected by the downwind radiation exposure," Barlow said. "And so a lot of our own referrals are word of mouth from the neighbor or 'I heard you had cancer. Well, my mom got the downwinder, so you should look into it.'"
Barlow added that the older adults in her service population tend to respond better to in-person communication than online. She said the last time she was in the hospital for a procedure, at least ten different people came up to her to ask about RECA's expiration date: "Wherever the opportunity comes up, you use it."
She also recommends considering types of outreach beyond traditional TV, radio, and newspaper ads (although her clinic uses these too). She's had clients who learned about her clinic through their local library's website. Barlow said it's important to know the smaller communities you serve and learn how best to reach those populations. Intermountain Healthcare also put an ad for the RESEP clinic on the computer screensavers in all of its facilities for three months.
The Southwestern Utah RESEP clinic's outreach efforts were limited due to COVID-19, but Barlow said the cancer program doctors and nurse navigators were still able to identify patients and send information to the RESEP clinic. The clinic then reached out to each patient.
"You catch somebody at a very tender part of their life when they're diagnosed with a potentially life-threatening diagnosis, like cancer," Barlow said. "And our goal is: whatever we can do to help them or make it easier for them, then we try and do it."

