Aug 09, 2017
Bringing Change for Rural COPD Patients: Possibilities with the COPD National Action Plan
This is the first of a two-part series focused on lung diseases in rural areas. Read part two – Pulmonary Health in Rural America: Cause and Impact of Work-Related Lung Diseases
Despite this rural divide, rural death rate trends for cancer, heart disease, diabetes, all are going in the right direction. Except for one chronic disease. That exception is COPD. This must change.
A January 2017 report issued by the Centers for Disease Control and Prevention (CDC) demonstrated that rural mortality rates have "decreased at a much slower pace, resulting in a widening gap between rural and urban mortality." But, COPD Foundation president Grace Anne Dorney Koppel is quick to highlight an important outlier disease.

"Over the past 15 years, there is this growing divide between rural and metropolitan America, especially for the five leading rural causes of excess deaths," Koppel said. "Despite this rural divide, rural death rate trends for cancer, heart disease, diabetes, all are going in the right direction. Except for one chronic disease. That exception is COPD. This must change."
Chronic obstructive pulmonary disease, or COPD, is the third leading cause of mortality in the United States, with nearly 150,000 deaths every year. In a 2015 American Thoracic Society abstract, Johns Hopkins researchers reported a national prevalence rate of 7.2%, but a prevalence rate of 11.9% in "rural-poor communities."
State-level prevalence data has been determined by CDC surveys. In 2013, an estimated 15.7 million people said they were told by a healthcare provider they had COPD, according to one CDC report. Experts and researchers worry that number may represent over-diagnosis. But they are also worried about another huge group of the undiagnosed — likely numbering up to 12 million or more — who possibly have the disease and don't know it, perhaps from under-recognition of the disease or due to a lag time before shortness of breath and cough impact daily activities.
With this substantial disease prevalence comes substantial healthcare costs. According to the Agency for Healthcare Research and Quality [report no longer available online], 2013-2014 expenditures for COPD and asthma reached nearly $77 billion, with inpatient costs nearing those of cancer.
What is COPD?
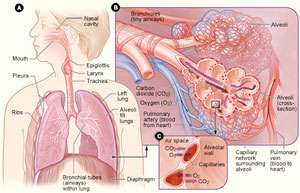
The CDC defines chronic lower respiratory diseases (CLRD) as chronic diseases of "airways and other structures of the lung." CLRD includes chronic obstructive pulmonary disease, or COPD, again with a COPD definition referring to the "group of diseases that cause airflow blockage and breathing-related problems." Often clinicians use "COPD" when referring to the end stages of multiple categories of lower respiratory diseases. Note: According to another CDC report, the most recent International Classification of Diseases, ICD-10, has reclassified COPD as CLRD.
But, prevalence and expenditures are only two aspects of
the COPD story. As Dorney Koppel points out, the looming
statistic is the mortality rate that occupies third place
on America's cause-of-death list and a rural death rate
that's even higher. A
2014 report by the Rural Health Reform Policy
Research Center shows the disparity to be most pronounced
among men, among whom the death rates "were 53 percent
higher in nonmetropolitan counties than in large
metropolitan counties in 2008-2010."
Changing Things: COPD Gets an Action Plan

For Dorney Koppel, driving change means sharing her own COPD story, a story that begins 16 years ago with significant shortness of breath unrecognized as COPD by healthcare providers. It's a story that exemplifies what can be done — and what still needs to be done. A national action plan can be the start to gearing up efforts needed to make a difference for COPD, a disease which she describes as both a life sentence and a death sentence.
"It's a death sentence because there is no cure, and they are decades away from finding one," she said. "And it's a life sentence because you are going to live with this disease until your final day. But, there are breathing techniques you can learn in pulmonary rehab. We have inhalers. We can learn to live better with this disease."
In May, the National Heart, Lung, and Blood Institute (NHLBI), in official partnership with the CDC, released the COPD National Action Plan. The plan, referred to as CNAP, has Congressional roots. In 2012, the Senate Appropriations Committee requested that the NHLBI and the CDC begin a response plan to the growing COPD problem. In 2014, Congress's COPD Caucus members sent a letter to the two agency directors again urging the creation of a national action plan. The NHLBI held several public planning meetings between 2013 and 2016, with final release of the plan in May 2017. Built on a framework of five main goals, CNAP's opening statement emphasizes one of the primary objectives, COPD awareness, since "many Americans are not aware of the significance of COPD as a major national health concern."
Dr. Antonello Punturieri, a program director at NHLBI, said that after the final draft was completed, public comments opened.
"Those were really, really sensational," Punturieri said. "The response was great. From single interested individuals to organizations and industry, we feel like we've got full stakeholder representation, including even those few who explained why they were withholding their support. And along the way? Well, the plan got better."
Acknowledging that rural populations represent areas of significant health disparities, Punturieri said that CNAP's rural touchpoints were important components of the plan.
"We don't cure this disease, but we've made progress in treating it, and we can make people feel much better," he said. "But looking at the rural data we have, rural areas haven't been reached. We've got to do something. We will really need local data, and we have to have rural partners to make this happen."
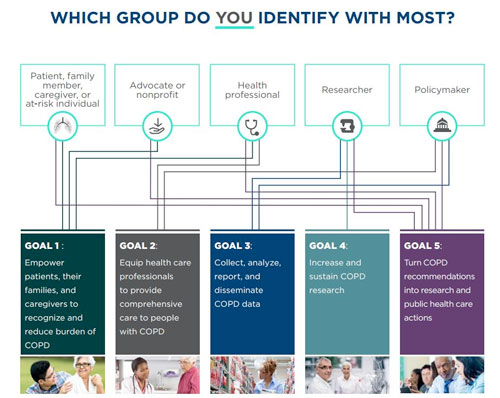
As Punturieri suggested, "action" was not just part of the plan's name but inherent in the plan's creation. Active participation for draft versions came from nearly 100 supporting organizations in addition to many other federal agencies, including the Federal Office of Rural Health Policy. The final plan clustered stakeholders into five main groups: policymakers, researchers, health professionals, advocacy and nonprofit organizations, along with patients, families, and caregivers. In the end, the NHLBI and CDC agency directors announced that the completed plan should be considered a "blueprint for a multi-faceted, unified fight" against COPD. Rural members identifying with several of these CNAP stakeholder groups said they see potential for collaboration and innovation to improve statistics and care delivery to rural COPD patients.
COPD National Action Plan's Rural Touchpoints
Goal 1: Empower patients, their families, and caregivers to recognize/reduce burden
Goal 2: Equip healthcare professionals to provide comprehensive care
- Subgoal 5: Improve access to care, including "hard-to-reach" areas
Goal 3: Collect, analyze, report, and disseminate data
-
Subgoal 1. a. iv. Surveys/studies include:
- At-risk populations
- Rural as well as urban populations
- Demographic factors including access to care
Goal 4: Increase and sustain research
- Subgoal 1. a. iv. Implement effective, widely accessible public health approaches to diagnosis and treatment
- Subgoal 5. a. Investigate impact of access to care
-
Subgoal 5. a.iii. Conduct research
identifying most effective structure and components
of a pulmonary rehabilitation program including:
- Most effective length and number of sessions
- Effects of different educational components and delivery strategies
- Effective ways to provide rehabilitation in rural areas
Goal 5: Turn recommendations into research and public healthcare actions
Rural Academic and Public Health Researchers
With research experiences ranging from cattle yard dust exposure, to current research involving rural patients with COPD, Dr. Tricia LeVan, Associate Professor at the University of Nebraska's College of Public Health, said she appreciates CNAP goals relating to research. Noting that the creation of COPD patient registries is listed under not one but three of CNAP's goals, LeVan said if healthcare delivery organizations caring for COPD patients can make registries happen, research on the disease could expand.
"Having a registry of COPD patients with demographic, accurate spirometry [lung capacity] and symptom data would help track COPD trends and address some of the goals of the CNAP," she said. "That would allow us to do epidemiologic-based research that is more translatable to patient care. Registries with high quality data can be challenging to create, but they are invaluable for patient care research, similar to cancer registries."
LeVan said she also appreciated CNAP's emphasis on multidisciplinary research collaboration. Taking research results from basic science and pairing it with other research approaches, like patient interventional studies, will help shed light on the unique rural aspects of the disease, she said. Especially when it comes to understanding that COPD is not just a smoker's disease.
"For many, many years, COPD was thought about as a smoking-only related disease," LeVan said. "That's not the complete story, as rural exposures, such as farm dust and smoke from wood burning stoves also contribute to COPD. And, interestingly, that concept is better accepted internationally than in this country, where COPD is a major health problem in rural and urban areas."
NHLBI's Punturieri was also emphatic about this point. He said it's very important to recognize that 20-25% of COPD cases are not due to cigarette smoking. He highlights other rural occupational lung diseases, some developing into COPD or COPD-like conditions over time. These, he noted, will need research attention also.
Even though the prevalence is lower than previous years, our rural kids are still smoking at nearly twice the percentage of their urban peers.
Though emphasizing that sensitivity must be employed to avoid stigmatization, Dr. Alana Knudson, co-director of the NORC Walsh Center for Rural Health Analysis, said that the rural smoking connection with COPD can't be ignored. Knudson points out concerning statistics related to rural smoking behaviors.
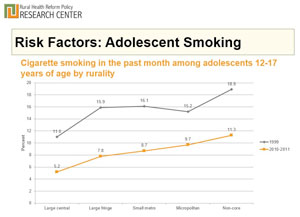
"What's most disturbing to me is the smoking prevalence among our kids," Knudson said. "Even though the prevalence is lower than previous years, our rural kids are still smoking at nearly twice the percentage of their urban peers. When you begin to roll that out over the next thirty, forty, and fifty years, we'll see these COPD disparities grow."
CNAP's Goal 5, turning research into public health action, is where rural researchers like Knudson can help provide insight for potential CNAP deliverables.
"Twenty years ago, there was little difference between urban and rural smoking percentages," Knudson said. "These recent data show increasing rural and urban differences in smoking behaviors may reflect the decreasing levels of funding allocated for rural public health programs – these types of risk behaviors, such as smoking, are often responsive to public health prevention measures."
Rural Clinicians and Healthcare Organizations
Supporting the CNAP emphasis on pulmonary rehabilitation (PR), family medicine physician Dr. Dan Doyle said that, despite caring for COPD and Black Lung patients for 35 years, he was late coming to full understanding of what PR offers.
"I've worked with COPD patients my whole professional life," Doyle said. "And only in the last several years have my eyes opened to the importance and value of pulmonary rehab. It doesn't use high tech. It doesn't use big drugs. It's a human relationship type of intervention. And patients don't just exercise, they get an education."
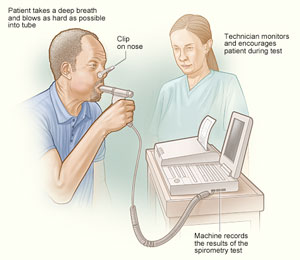
Doyle, the medical director of two PR facility sites associated with the Grace Anne Dorney Pulmonary Rehabilitation Project of West Virginia, said that having these rehab facilities in their Federally Qualified Health Centers has brought three important dimensions to clinic-based COPD patient care: specialized instruction in physical activity and disease education; improved spirometric testing and data collection to monitor progress and outcomes; and employment of respiratory therapists, the healthcare professionals who not only have a skill set assisting with all types of COPD therapies but who also have a passion for patient education. As the lead author on the sole current paper looking at rural pulmonary rehab program implementation and outcomes, Doyle also adds that this education is not just for COPD patients. These therapists help other patients with chronic lower respiratory conditions, some of which eventually evolve into COPD or COPD-like diseases.
In Zanesville, Ohio, Genesis Healthcare System's COPD team had been waiting for the action plan's final release. Mari Varhola, registered nurse and manager of Genesis's Lung Clinic and Pulmonary Nurse Navigators, said their team is looking forward to the innovation that the action plan might bring to their current patient care models. Varhola said their COPD 30-day readmission project has received national attention, and she fielded a recent call from one of their state's large academic research center. They're very proud of what they are currently doing, but they have a culture of innovation to better care for their patients.
"For example, we've got some current work centered in a continuum program, looking specifically at where the COPD process starts," Varhola said.
She said she was pleased to see the attention that CNAP's Goal 1 brings to families and caregivers. She said she is constantly thinking about ways to better serve this group and wonders how they might collaborate with others having similar objectives.
"The family members who provide transportation, taking off work to help make appointments, who sometimes end up paying for medications, or the stress that family members experience from living with a patient and being unable to get them to stop smoking, that's a big piece of COPD that's not always addressed," Varhola said. "And these caregivers need more than the pamphlet they're often handed."
Perspectives from Other Stakeholders
The rising prevalence of COPD in women, which includes women in rural areas, is a focus for the American Lung Association, another stakeholder. Their awareness program, Taking Her Breath Away, brings attention to this population included under CNAP's third goal. Dorney Koppel also speaks out in the campaign's opening remarks: "Sadly, COPD is now a disease in which women have reached a grim parity with men…since 2000 the disease has actually claimed the lives of more women than men in this country each year."
Dr. MeiLan Han, a spokesperson for the Association, is a practicing pulmonologist, physician educator, and researcher – and she is no stranger to the challenges for rural COPD patients. She grew up in rural Idaho and received her medical education through the University of Washington's WWAMI and its specific programs.
"As a spokesperson, I can speak out and advocate for COPD patients, patients who have unique needs as compared to other chronic diseases," Han said. "And unfortunately in many instances, particularly for those living in rural areas, these needs are not being met. These patients are also uncomfortable speaking up for themselves because they feel stigmatized as they believe the disease is seen as self-inflicted."
Han also points out that, until all five stakeholder groups get involved with CNAP implementation, the plan is just that: A plan.

"Some solutions for COPD patients will need to be the result of creative action, and some will require legislative action," she commented. "But key to this will be earmarking funding to carry out the CNAP. We have to make some noise about COPD to start making a difference."
Dorney Koppel also raises funding awareness when it comes to COPD solutions. During public presentations, she clarifies this solution by sharing one fact: Despite its location in the top three leading causes of death, current COPD funding is much less compared to other disease categories with much lower death rates.
CNAP's Primary Stakeholders: It's All about Patients
Though her approach to making a difference starts with sharing her personal story, Dorney Koppel said she's really inspired by the stories of rural patients she's met. But, she remains troubled that, despite the sheer number of patients, the condition is largely unrecognized by many individuals who fall into stakeholder groups.
"There is ignorance about the devastating consequence of this disease that is so pervasive," she said. "It's not just in rural America, it's metropolitan America, it's academic America. Even within the medical profession, there are people who don't have current information about what can be done for COPD."
She said her personal story as well as her awareness activities has led her to identify with all five stakeholder groups. She understands policymakers. Through the COPD Foundation and the Dorney-Koppel Family Foundation, she and her husband, Ted, have track records with advocacy groups, researchers, and clinicians. They've worked with rural stakeholders: By year's end, their foundation will have assisted in establishing 10 pulmonary rehabilitation centers, 9 of which are in areas of rural America where the disease has a higher prevalence.
And in rural America, where the distances are greater from getting care, patients can be trapped in their homes, unable to breathe, unable to move. Working together, we must make a difference for them.
"What's often overlooked is the despair and isolation associated with this disease," she said. "Many people struggle all day long, trying to take just one deep breath. And in rural America, where the distances are greater from getting care, patients can be trapped in their homes, unable to breathe, unable to move. Working together, we must make a difference for them."
Planning for COPD Awareness Month
Rural communities and healthcare organizations may find these resources helpful for November's COPD Awareness Month and November 15, World COPD Awareness Day:
American Lung Association
COPD Foundation
National Heart, Lung, and Blood Institute
Academic Publications
For further understanding of pulmonary rehabilitation program benefits, listen to patients share their experiences:

