Aug 11, 2021
Understanding the Rural Swing Bed: More than Just a Reimbursement Policy
 In the 1970s, expert observers noted that
rural America had the wrong number of beds dedicated to
the wrong level of care. Rural hospital beds were empty
because patients were being referred to urban centers for
acute tertiary care treatment. Needed nursing home beds
for post-acute care had disappeared, mainly due to
regulatory changes and a pervasive sense of "business
pragmatism" that surrounded reimbursement policies.
In the 1970s, expert observers noted that
rural America had the wrong number of beds dedicated to
the wrong level of care. Rural hospital beds were empty
because patients were being referred to urban centers for
acute tertiary care treatment. Needed nursing home beds
for post-acute care had disappeared, mainly due to
regulatory changes and a pervasive sense of "business
pragmatism" that surrounded reimbursement policies.
As unbelievably dire as the bed situation was back then, today's experts point to the problem's almost-as-unbelievable simple and effective solution: the swing bed.
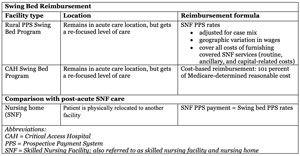
According to the 2020 CMS interpretive guidelines for swing beds in Critical Access Hospitals (CAHs), "a 'swing-bed' is a change in reimbursement status." As a payment model, then, a CAH can use its beds interchangeably for either acute care or post-acute care. The reimbursement "swings" from billing for acute care services to billing for post-acute skilled nursing services, despite the fact that the patient usually stays in the same bed in the same physical location.
As the program enters its fifth decade, experts pointed out that rural hospitals have been able to keep serving their communities because swing bed programs often contribute to a positive operating margin. A local swing bed program also directly impacts local rural residents: As a patient-centric post-acute care solution, rural patients who find themselves too well to stay in the urban hospital but still too sick to go back to their own homes can return to their rural community hospitals for further care.
Swing Bed Model of Care: The Early Days
The swing bed was a solution offered by Dr. Bruce Walter, a physician who was Utah's director of Medicare services back in the late 1970s and early '80s. Walter's swing bed concept, with its six potential reimbursement options, was a model he envisioned to be "utilized in small hospitals, urban and rural, across the country."
"Such a program nationwide should not be measured merely in terms of balance sheets and occupancy percentages," he went on to say in a 1980 publication, "but also in terms of personal benefits gained by patients and their families."
John Supplitt, the American Hospital Association (AHA) senior director for Rural Health Services, first came to AHA in 1981 as its swing bed project director. He described what many experts expressed as the essence of the program.
"The reality was that the swing bed program provided a way to maximize the use of existing resources and to take those assets and employ them in a manner that was best suited for the patient and the organization in a way that allowed the healthcare organizations to maintain their clinical relationship with the people who resided in those communities," Supplitt said.
He also emphasized that, in addition to offering essential clinical transitional care services, this pioneering model of patient-centric care is now linked to a reimbursement model unique to both the rural PPS (prospective payment system) hospital and the CAH — a hospital designation that didn't exist prior to 1997 — that effectively nudged "business pragmatism" out of the rural post-acute care attitude.
Swing Bed Impact

Experts emphasized that in the world of health service delivery, few models exist that serve patient, hospital, and community as well as the swing bed program does. Supplitt highlighted the patient-centric philosophy that is core to the program.
"What inspired and drove swing beds was the patient-centered approach to care and the ability to coordinate that care at different levels," Supplitt said. "From inpatient acute care through discharge to post-acute swing bed care, the ability to maximize our resources — both human and our physical assets — and address some social determinants of health, these were really the foundation of what this new model of care and new model of payment represented."
Tim Wolters, a financial and reimbursement expert for small, rural, and Critical Access hospitals in Missouri, pointed out that, for many patients, having a swing bed program keeps their post-acute care local — a benefit not just for patients, but their families and their communities.

"Some hospitals may not even have a long-term care facility in their area," Wolters said. "If they don't have a swing bed program, that patient may have to be moved 30 or 50 miles away to another community for their post-acute care. That's where the swing bed program really comes in as a valuable resource."
Experts also pointed out that another patient-centric benefit directly linked to the swing bed program is the rural hospital's bed staff's professional skills. Ralph Llewellyn, a rural hospital financial consultant and previous small rural hospital CFO, said that because the swing bed is a designation for billing only, the patient usually remains in the same bed in the same location with the same staff who provided their acute care. However, that same staff has expertise often not found in alternative post-acute settings, like nursing homes.

"We understand that the swing bed has the same 3-day qualifying requirement as skilled nursing home care," Llewellyn said. "But there are certain things that sometimes aren't done in a nursing home setting either because it's a high-cost item or involves processes done in too small numbers for staff to have needed proficiency — for example, infusions. Because the swing bed is located within the hospital, you will have nurses who do infusions all the time. It's second nature to them. Therefore, the swing bed provides service levels that might otherwise not be done in the community. If the program were not there, patients would have to relocate from their local community to get those services."

In addition to its patient-centric focus, the swing bed program brings value to its rural community. Joanie Perkins, Chief Compliance Officer at North Sunflower Medical Center (NSMC), Ruleville, Mississippi, shared the community-centric philosophy of her organization and said that both the immediate community and surrounding communities depend on NSMC for post-acute care.
"We are the hospital of choice for swing bed services in our area and we have a lot of people come to us," Perkins said, further explaining that the organization's volume is also a product of its large Rural Health Clinic with extended hours. "We sort of sell ourselves around the message that we're going to take care of you here, where your home is. We're going to take good care of you here. Our average length of stay might be a bit longer, but it gives us a longer period of time than available in the acute care setting for the patients to really engage with their therapy staff and their nursing staff."
CAH Swing Bed Impact
Patient-centric:
- Subacute care close to home
- "Right care in the right place at the right time"
- Little restriction on medical complexity
- Continuity of care in same bed/with same staff
- Enhanced transitions of care
- Enhanced services (example: infusion therapies not available in skilled nursing facilities)
- Completion of subacute phase of an episode of tertiary-level acute care
- Avoids patient-perceived stigma/fear associated with traditional nursing home care
Hospital-centric:
- Stable staffing schedules: Flexibility between acute/subacute care beds avoids low-census canceled staffing
- Probable decreased readmission rate
- Reimbursement structure promotes sustainability of acute care services
- Showcase community commitment
- Emergency preparedness flexibility (example: COVID-19 surge)
Community-centric:
- Hospital as a financially stable economic community member
- Brings additional services that also serve outpatient populations (example: therapies such as physical and occupational)
- Cost-effective alternative to constructing alternative forms of long-term care
Understanding PPS Hospital and CAH Swing Bed Reimbursement
Experts were frank: There are so few relevant negatives linked to the swing bed program that focus should remain on the less understood positive aspects — for example, reimbursement.
Wolters said that swing bed reimbursement is key to understanding the program's benefits.
"On the PPS hospital side, the most important aspect of reimbursement is that it is just a better way to manage the care of the patient: Patients get the appropriate level of acute care with the DRG [Diagnostic Related Groups] payment," Wolters said. "When the patient no longer needs the acute level of care, they can move to swing bed care and the facility still gets some additional payment for that post-acute care.
"Understanding how the reimbursement works for the Critical Access Hospital is also important," he said, further explaining that for CAH reimbursement, costs are more a factor related to how many patients are in both the acute care and swing bed designation at any given time. "A simplistic example is this: If a hospital has additional patients in the swing bed program, that reduces the cost of care on the acute care side, too. For most of these hospitals, their staffing level is relatively fixed, so if the hospital has nursing costs of $X on a calendar day and they have only one acute care patient in the hospital, then that hospital's care cost is $X. If they add a swing bed patient and they now have two patients, then that swing bed patient cost is one-half $X, which might seem exorbitant until you understand that now the total cost of that facility's care per patient is actually one-half $X per patient."

Describing another benefit of the swing bed program, Roger Knak, CEO of Fairview Regional Medical Center, in northwest Oklahoma, said that their swing bed program stabilizes the organization's cash flow. Serving over 7,700 people in a 5-county area, the hospital averages a low acute care census and its swing bed program not only provides a dependable revenue stream, but the region's patients can get their care locally.
"We can't always justify transferring patients upstream after 72 hours," Knak said, emphasizing that after 3 days, often a patient's treatment plan transitions to a lower level of care that is appropriate for a short swing bed stay. "Quite honestly, those upstream organizations often don't have the capacity to accept these patients anyway. The ability to provide this post-acute care in our local swing bed unit stabilizes the census for better staffing efficiency and provides a consistent cash flow."
Mississippi's Perkins said she is clear about the swing bed program's financial benefit for their hospital — and the fact that it is especially strategic for their community located within the Delta region, which she pointed out has had an alarming number of hospital closures and at-risk organizations, as this 2019 North Carolina Rural Health Research Program (NCRHRP) findings brief (no longer available online) highlighted.
Without swing beds, we'd be just another one of those closed hospitals in a little, tiny Delta town that people go, 'Wow, and that's over.'
"Without that swing bed program in our hospital, we would not exist today," Perkins said. "At one point back in 2005, people were giving part of their paychecks back to keep this hospital open. Then a new CEO arrived and converted the organization to a Critical Access Hospital, convinced a great group of primary care providers that our swing bed program could be an appropriate place for their patients to do their rehab, and we developed a really robust rehab department. Without swing beds, we'd be just another one of those closed hospitals in a little, tiny Delta town that people go, 'Wow, and that's over.'"
On Another Reimbursement Front: Reimbursement Simulations, Quality Measurements, and Demonstration Projects
As indicated by Perkins and Knak, swing bed revenue is important for CAHs' operating margins.
According to a 2019 Illinois report analyzing a CAH network's swing bed program, revenues accounted for over 20% of total inpatient revenues for 35% (17 of 48 responding CAHs). Additionally, for nine of those respondents, swing bed revenue actually accounted for more than 30% of total inpatient revenues.
Researchers have used reimbursement simulation to explore what might happen with changes in CAH reimbursement. A NCRHRP report from 2020 (no longer available online) stated that "eliminating cost-based reimbursement could substantially increase the pressure on already vulnerable rural hospitals," especially in the South.
Further linking future potential reimbursement changes to quality reporting is a task currently not mandated for CAHs but will likely be essential to any conversation regarding change to the current reimbursement mechanism.
Rural researchers spotlighted another impact related to policy. In a 2018 report, the Rural Policy Research Institute (RUPRI) pointed to unintended consequences of the 2014 legislation Improving Medicare Post-Acute Care Transformation Act (IMPACT). Though intended to decrease paperwork for rural organizations already stressed with lack of workforce, instead it might have created an unintended financial threat to patient care access to swing beds. The researchers stated, "CAHs with swing beds may not be selected for post-acute care services due to the inability of acute care providers to judge their quality. CAHs with swing beds that are bypassed for post-acute care stays because of a lack of quality reporting are missing an important opportunity to add financial stability and provide essential post-acute care health care services locally."
Financial expert Llewellyn said there are strong arguments for doing the work of quality monitoring.
"I'm a very firm believer in rural America and the ability to deliver quality," Llewellyn said. "The challenge is that people on the outside can easily say, 'They're [CAHs] just not really taking care of complex patients,' or 'They're not providing quality.' If we don't have quality markers, we can't prove complexity and by not being able to prove complexity, we can't prove that the delivered care is cost-effective."
Quality Measure Research by the Rural Health Research Centers
 In addition to addressing
many aspects of swing beds over the years, the
Rural Health Research Centers, funded by the Federal
Office of Rural Health Policy, have also specifically
explored the need for quality measures and have ongoing
research efforts on nursing quality measures for swing
beds.
In addition to addressing
many aspects of swing beds over the years, the
Rural Health Research Centers, funded by the Federal
Office of Rural Health Policy, have also specifically
explored the need for quality measures and have ongoing
research efforts on nursing quality measures for swing
beds.
Already involved in quality reporting activities because
of her Mississippi organization's Rural Health Clinic and
recent involvement in the early development stages of a
statewide Accountable Care Organization, Perkins said she
is adamant about the need for quality reporting.
"It is my personal wish that they mandate quality reporting," she said. "I would love to see the State Offices of Rural Health or hospital associations get together and come up with some really good quality measures that make sense for all of us and get this rolling. I don't see why we should sit back and wait. Do you think quality is going away? We're going to be paid for our performance and it's all going to be about the quality of care."
In Oklahoma, Knak's swing bed program is involved with a joint replacement bundled payments initiative because most of their local patients have the procedure in a metro area but often return to Fairview's swing beds. He said that this bundled payment model forced several changes in their swing bed program: a lower swing bed census because some of the participating patients were discharged directly home but included quality monitoring that has actually proved the program's excellence.
"When our local patients followed up, their orthopod in the city would say, 'Well, you're weeks ahead of where I expected you to be because your therapy's doing so well,'" Knak said, explaining that his organization's swing bed program and therapy department has gained tremendous respect in metro Oklahoma. "Based on outcomes and costs, the orthopedists would like to send more of their urban clients to our facility for rehab, but the hesitancy of those patients makes it almost impossible since they'd be away from their families. There's also the mindset that rural is backwards. But when you look at quality outcomes, it's just the opposite. The quality outcomes in a rural environment are often much higher than the urban environment."
Swing Beds and Medicare Advantage Plans
With their participation in the bundled payment initiative, Knak said that lack of contractual agreements with Medicare Advantage (MA) plans has also challenged his organization's ability to get their local patients back to their swing bed program.
"We don't have every contract and we can't afford every contract because instead of paying us cost-base, they're paying us at a nursing home skilled care rate which is significantly less," Knak said. "In the 'olden days,' everybody knew they had 100 days skilled care and swing bed care. Now when I say, 'You don't qualify for that,' they ask, 'Well, why not? I've got my Medicare.' Then we explain their plan is an Advantage plan and not traditional Medicare."
Backed by a 2019 RUPRI report (no longer available online) indicating a growing rural enrollment in these plans, financial expert Wolters shared additional MA plan experiences that he said he thought were particularly important to rural swing bed providers.
"Though it varies around the country, in our market we are seeing more and more penetration of Medicare Advantage plans," Wolters said. "This can be disadvantaging to rural hospital swing beds as traditional Medicare transitions to more Medicare Advantage. I've seen a negative financial hit in certain circumstances. It really is important for the hospital to monitor that and make sure they're getting paid appropriately for their care. While Medicare does require these plans to pay the same per se, the plans frequently limit reimbursement to actual charges, which is often less than Medicare's payment rate. They need to clarify that when they say, 'We pay the same,' they mean they pay the same."
Swing Bed Model: Need for Future Modification?
In generalities, Supplitt, Llewellyn, and Wolters all agreed: The swing bed program needs only minor modification from its current model. Each expert offered additional thoughts on the current and future version of the enduring model first conceptualized by Walter so many decades ago.
Supplitt emphasized that in addition to providing a reimbursement "lifeline" allowing rural hospitals to continue medical services for their communities, the swing bed program also creates a local post-acute care solution. In addition to those two benefits, he said that with COVID-19, the program also proved itself an invaluable public health emergency (PHE) response tool for both urban and rural residents: When urban post-acute beds were at capacity, many anecdotal reports noted that patients were transferred from urban hospitals to rural swing beds. He said these beds were also integral to managing rural surge capacity management within an individual organization, and sometimes patients were transferred between rural organizations themselves.
Swing bed as an in-place PHE response tool proved itself an important part of COVID-19 emergency response.
"Swing bed as an in-place PHE response tool proved itself an important part of COVID-19 emergency response," Supplitt said. "When we look at the administrative waivers granted under the public health emergency declaration, what we saw was how important flexibility is in terms of being able to step up in a disaster of this magnitude to meet demands cascading in on both hospitals and clinicians themselves. Removing some of the regulatory obstacles proved fortuitous and the flexibility essential in terms of being prepared for disasters."
A concern raised by Llewellyn involves the problems associated with the 3-day qualifying stay for admittance to the swing bed program. He said it's confusing for patients and providers and — very possibly — an artificial barrier to getting the patient into the right level of care at the right time.
"The 3-day qualifying stay was waived for the COVID-19 public health emergency and it'd be interesting to see how those waivers have played out," he said, noting that specific research around the waiver would be valuable for payers and those who deliver post-acute care.
In addition to keeping up with the clinical direction that remote patient monitoring is bringing to allow more and more acute and post-acute care at home, the future of swing beds certainly could benefit from further research, Llewellyn suggested.
"The data doesn't exist to prove things such as quality and the program benefits," he said. "There is a lack of data around the complexity of the individuals that we're caring for and that lack of data creates challenges. People on one side say, 'It's expensive. We should change it up.' The other side says, 'It's high value.' The truth is somewhere in between."
Lastly, Wolters added that it's important to not lose focus on the value swing beds offer in terms of managing the growing population health issues of the increasing numbers of older rural residents.
More and more patients may choose to stay close to home when they can, and swing beds need to continue to be a viable option to the fullest extent possible across rural America.
"We see the population aging," Wolters said. "I look in the mirror every morning and see that happening. We need to make sure all appropriate acute and post-acute care options are available to rural patients. More and more patients may choose to stay close to home when they can, and swing beds need to continue to be a viable option to the fullest extent possible across rural America."

