Mar 21, 2018
Understanding the Science of Pain and Opioids
Back to What's MAT Got to Do with It? Medication-Assisted Treatment for Opioid Use Disorder in Rural America.
What Is Pain?
 A well-accepted
pain definition comes from the International
Association for the Study of Pain: "Pain is an
unpleasant sensory and emotional experience that
is associated with actual or potential tissue damage or
described in such terms."
A well-accepted
pain definition comes from the International
Association for the Study of Pain: "Pain is an
unpleasant sensory and emotional experience that
is associated with actual or potential tissue damage or
described in such terms."
Experts agree pain has no objective measure and no easy treatment.
How Do Opioids Work?
Opioids don't have any direct impact on the body area that hurts or is injured. They don't attach to a broken bone, or to a decayed or infected tooth, or the incision from an operation. Unlike medications such as ibuprofen, they don't decrease inflammation that often causes pain. Instead, when an opioid is taken as a pill, injected into a vein, or even smoked, it travels through the blood stream and relieves pain by acting on the brain. Once in the brain, opioids influence the way the brain thinks and feels about an unpleasant sensation. According to the National Institute on Drug Abuse (NIDA), here are three specific brain areas where opioids have influence:
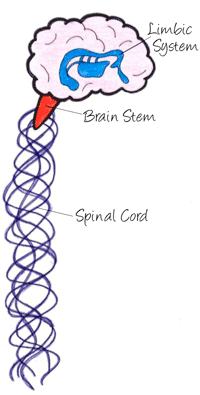
| Brain Area | Daily Function | Opioids' Influence |
| Spinal cord | Transmits sensations from different body areas to the brain. | Dulls the pain sensation once it reaches the brain. |
| Brain stem | Controls the body's automatic functions like breathing, the heartbeat, and even some elements of speech. | Slows or even stops breathing. Lessens coughing. But, here is where opioids can even stop the brain from registering an unpleasant sensation. |
| Limbic system | Controls positive and negative emotions, mood, learning, and memory; it also houses the brain's "reward circuit": structures that control and regulate pleasant feelings. | Creates feelings of pleasure, relaxation, contentment. |
The National Institute on Drug Abuse's Brain Disease Model of Opioid Use Disorder: Reward Gone Wrong
Dopamine is a brain chemical that influences the brain's reward circuit. This circuit craves behaviors that give pleasure, like engaging with friends, or behaviors that keep us alive, like eating.
Opioids trigger a "dopamine flood," and the reward circuit experiences an intense, exaggerated sense of well-being, called euphoria. With continued opioid use, the reward circuit doesn't want anything to stop that dopamine flood.
Meanwhile, the brain realizes it can't tolerate that constant dopamine flood. Eventually it decreases dopamine production: less dopamine, less flooding, less pleasure. The brain becomes depressed, flat, and lifeless. But the reward circuit still craves euphoria. The new norm? A brain that can't experience joy, euphoria that can't be reproduced, and craving in the reward circuit that has no brakes: the reward circuit gone wrong, creating the brain disease that is opioid use disorder, a complex disorder that is also influenced by various genetic and psychosocial factors.
|
Who is at highest risk for opioid misuse?
* Adverse childhood experiences are also recognized as a significant risk factor for developing substance use disorders. Source: Opioid Risk Tool |
Other drug misuse risk factors:
Source: NIDA's Science of Addiction |
 According to the Substance Abuse
and Mental Health Services Administration (SAMHSA)
webpage [no longer available online], "in 2014, an
estimated 1.9 million people had an opioid use disorder
related to prescription pain relievers."
According to the Substance Abuse
and Mental Health Services Administration (SAMHSA)
webpage [no longer available online], "in 2014, an
estimated 1.9 million people had an opioid use disorder
related to prescription pain relievers."
It's difficult to determine the exact number of rural residents with OUD, but experts say there are proxy data. Proxy measures might be found in county-level overdose data since those fatality numbers perhaps represent many who might have benefited from MAT. Proxy numbers could be found in nonmetropolitan drug-related incarceration rates or patient numbers presenting to emergency rooms requesting refills for lost prescriptions. Proxy numbers can be tracked by using a state drug monitoring program which collects opioid dispensing information. Or maybe OUD patients are among a clinic's established patients who present for pain out of proportion to a normal physical exam, with vital signs and history suggestive of opioid withdrawal. Proxy numbers might even include patients who finally say "I need help."

