Aug 07, 2019
Mobile Telehealth Units and Care Coordinators Improve Emergency Care Services for Rural Arizona Patients
by Jenn Lukens
 When Summit Healthcare
Association in eastern Arizona began experiencing a
steady increase of emergency room (ER) readmissions, it
was clear something needed to change.
When Summit Healthcare
Association in eastern Arizona began experiencing a
steady increase of emergency room (ER) readmissions, it
was clear something needed to change.
Summit's first focus was its emergency medicine process. Because many of its ER visits came from ambulance transports, Summit began exploring the use of telehealth technology as a means to provide real-time advice from ER doctors to first responders on the road. Their second focus was a natural next step: to improve the transitions of these patients into follow-up care that would ultimately lessen the likelihood of future ER visits.
In 2016, Summit formed a network and applied for the Rural Health Network Development Program (RHND) grant from the Federal Office of Rural Health Policy (FORHP) to help fund two services. First, mobile telemedicine units would allow first responders to transmit information and receive real-time advice from ER physicians. The anticipated effects were better triaging, advanced onsite care, and referrals to facilities that could best meet patients' critical needs. Second, follow-up and educational efforts from care coordinators would improve the transitions of patients with chronic disease and/or behavioral health needs to appropriate care.

In just the second year of the program, the Network for Improved Outcomes in Rural Emergency Care (NIOREC) program's healthcare interventions have proved promising, saving an estimated $1.2 million in air and ground ambulance transport costs by leveraging telemedicine to serve patients locally — providing the right care, at the right time, in the right place.
An Urban Telehealth Model Adapted for a Rural Setting
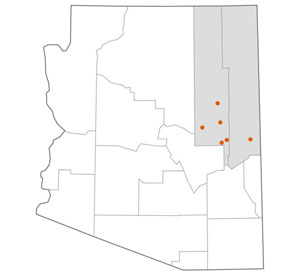
Based in the micropolitan town of Show Low, Arizona, Summit Healthcare Association includes a full-service medical center with an 89-bed hospital and five outlying clinics. All are located in southern Navajo and Apache counties, north of the White Mountain range.
The area's healthcare system already had significant telemedicine infrastructure in place when awarded FORHP's RHND grant. Summit began looking for a way to use its existing telehealth technology to link first responders to emergency department physicians. When they learned about a successful urban-based model, Summit leadership foresaw the benefits in applying the same principles within the rural Arizona community.
"It sparked inspiration for something we could do to leverage telemedicine, which would allow us to provide better support to EMS agencies in the field and, hopefully, look to build a model that will ultimately reduce ER visits that could be treated in lower-acuity settings, such as an urgent care or primary care office," said Kristi Iannucci, MBA, Summit's Telehealth and Lean Improvement Specialist.
Iannucci was hired to direct NIOREC shortly before the program launched. Her experience working with telehealth initiatives for a network partner allowed her to see the value of the project.
Although telehealth has been widely accepted and used to link one provider to another for medical advice, for emergency medical services (EMS) in rural America, it's still being tested. Complications with bandwidth, mobile units, and video imaging have been enough to discourage some facilities. But for NIOREC, the benefits far outweigh the challenges. "I think what we are trying to do with telemedicine is very forward-thinking. I totally believe that this is going to be the future of healthcare. It's exciting to be on the forefront of that," said Iannucci.
NIOREC was one of 51 rural recipients of the Rural Health Network Development Program and will receive close to $600,000 over the course of three years. So far, the funds have been used toward equipment, training, and personnel.
NIOREC Telehealth Services
The NIOREC program offers the following types of telehealth mediums to its partners:
- Real-time communication – Two-way connection and consultations are completed by phone or video.
- Store-and-forward – Information about a patient is recorded, stored, transferred, and accessed across distances.
- Remote patient monitoring – Providers can access patients' vital signs daily and record the data.
From the Ambulance to the Emergency Room
Summit serves as a base hospital for NIOREC EMS members, which include Timber Mesa Fire and Medical District, Pinetop Fire, Taylor-Snowflake Fire & Medical Department, St. Johns Emergency Medical Services, and the Heber-Overgaard Fire District. Together, they cover most of Summit's 3,330-square-mile service area. Iannucci attributed the program's smooth launch to the existing partnerships Summit had with these EMS agencies.
Through the RHND grant funds, Timber Mesa Fire and Medical District installed telemedicine equipment in one ladder truck, four fire engines, and five ambulances. Each vehicle now has a mobile broadband router that allows for cellular connection and high-speed internet access, cutting down on connectivity "dead zones." A 12-lead electrocardiogram (EKG) machine transmits heart functions via wireless broadcast to a shared, cloud-based storage site. This feature makes it much easier for an ER physician to immediately access the information, make a diagnosis, recommend a transfer, or prepare the medical equipment necessary to treat the patient upon arrival.
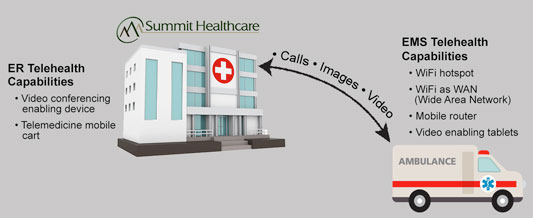
Because the units are mobile, first responders can activate their telemedicine systems while en route to a medical facility. An automatic vehicle locater allows the EMS vehicle to be easily directed to the nearest healthcare facility when necessary.
NIOREC Telehealth Communication Codes
A first responder calls in to a recorded line, known as a "patch line," using these three codes to communicate what has already been done and what is still needed:
- Activate the system – Information or images need to be sent to the ER via wireless broadcast for a physician to evaluate the patient remotely.
- Treat and refer – EMS is treating the patient onsite and transferring him or her to the closest medical facility.
- Transfer – EMS is transferring the patient to the nearest Summit facility.
Clint Peck, RN, is the Pre-Hospital Coordinator for
Summit and serves as the liaison between hospital and
first responders. "It's been an absolutely
wonderful thing having that early recognition and early
diagnosis," said Peck, specifying that having
12-lead EKG capability is a large contributor.
"Some of our agencies may have an hour
transport time just to get to this facility, so when you
have a critical patient in your ride, having the
capability of a physician to see that patient and give
you recommendations and orders on what you might do
differently prior to the patient coming — it is
a big thing for us in rural."
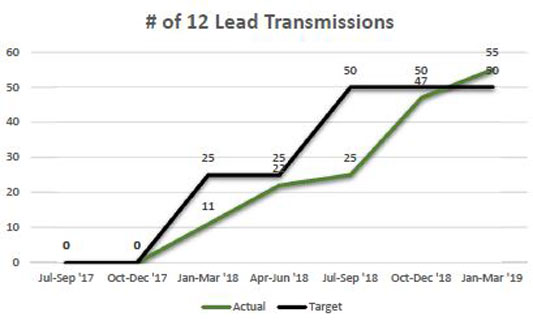
Prior to this program, the time it took to prepare a catheterization laboratory (cath lab) for a patient having a heart attack was upwards of 30 minutes. "But with this capability…everything is completely set up at the bedside before a patient hits the door," explained Peck.
The telemedicine video aspect of the mobile units is still being tested, but NIOREC plans on having it up and running later this year. Peck anticipates it will benefit all parties: "This program allows our ER physicians to actually have the capability to lay eyes on a patient, even if it's a patient who doesn't need to come to the emergency room and can be treated by a local urgent care center or another physician's office to help alleviate the overcrowding in our ER."
Care Coordinators Link Patients to Next Steps
The second focal point of the NIOREC program encompasses behavioral health needs of patients with chronic diseases. The focus has good reason: nearly 40% of Summit's patient population screen positive for depression, and 75% of patients with two or more chronic physical conditions have a comorbidity related to behavioral health.
Through the work of Summit's care coordinators, NIOREC links patients to services like behavioral health to address needs that may have contributed to their ER admission.

Ivy Loney, DBH, LMSW, is the Director of Integrated Behavioral Health at Summit. She manages the care coordinators, all four of whom are experienced registered nurses. Their credentials have been beneficial in triaging patients with behavioral health issues. "There is definitely fear around social services for patients in rural Arizona, so what we find is that some patients will flat-out refuse to talk to a behavioral health consultant, but they are more than happy to talk to a nurse care coordinator," she explained.
While Summit offers appointments with master's-level behavioral health providers, patients needing care that is more specialized are referred to ChangePoint Integrated Health, a community mental health clinic and crisis stabilization unit and NIOREC partner. Having ChangePoint as a place to refer patients in need of behavioral healthcare has contributed to NIOREC's goal to get patients the most appropriate care without having to be admitted to the ER. This year alone, 399 patients have been routed to ChangePoint from Summit, EMS, and outside referrals. In the future, the NIOREC program plans on having a crisis worker available for a video conference at the time of an EMS call.
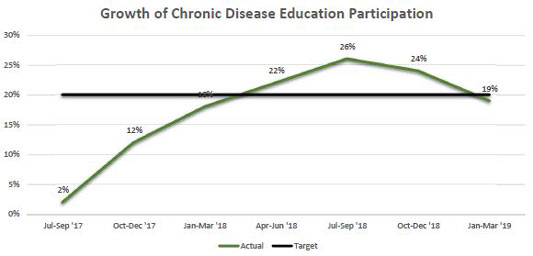
The work of Summit's care coordinators goes beyond behavioral health and encompasses outreach to every patient treated by telemedicine. Through a phone call following a telehealth episode, care coordinators ensure patients have a medication regimen and upcoming appointments scheduled. They also take time to educate the patient on their discharge treatment plan and chronic disease management. Virtual and in-person educational classes are also offered to patients with chronic conditions. So far, enrollment in these classes has reached a high of 26% of patients approached since the start of NIOREC.
Because of its impact on health outcomes and disparities, health literacy has become a priority for Summit's care coordinators in helping patients understand their diagnoses. For instance, clarifying the meaning of "congestive heart failure" could be the first time the patient hears their condition explained in layman's terms. "Many times, they don't understand the gravity of the diagnosis…and that's where we come in," explained Loney.
The program's care coordination efforts further employ telehealth services through the use of remote monitoring devices. Care coordinators offer one of these devices to patients transitioning back home who have qualifying medical conditions (congestive heart failure, chronic pulmonary disease, or severe diabetes). The device tracks vital signs and relays the results to the patient's medical care team. Care coordinators set up the device in patients' homes, taking the opportunity to educate them on its proper use and how the patients' vitals are connected to the numbers displayed.
"For instance, as blood pressure is elevating, they are able to realize, 'When I start to feel light-headed, that's when my oxygen level is going down.' They become more familiar with how those physical symptoms are being affected by those biometric markers," explained Loney.
The work of the care coordinators has contributed to an overall reduction in hospital readmission rates across the Summit system, which now stands at 4.22%, down from 5.55% in the first year of the grant program. And the rate of follow-up appointments with primary care after an emergency department discharge increased from 12% to 48%.
A lot of times, people get the impression that patients are noncompliant. It's not that they're noncompliant, it's that they need that support.
Although Loney would like to see even better outcomes, she said this is a good start. In addition to the improvements made, she views the initiative patients learn to take – like checking the status of their diagnosis, preauthorization, or medications – as the biggest success of the care coordination aspect of the NIOREC program: "A lot of times, people get the impression that patients are noncompliant. It's not that they're noncompliant, it's that they need that support."
Challenges, Sustainability, and Future Impact
While broadband connection is generally strong in the mountainous region, one barrier Summit had to address before launching the NIOREC program was getting partnering EMS vehicles connected. Summit contracted with two service providers to install mobile routers in the vehicles and enhance broadband accessibility for those routers. Partnering EMS agencies now have instant telehealth capability when treating or transporting a patient.
Another challenge was getting all first responders comfortable with the telemedicine equipment. Using a Train the Trainer model, representatives from partnering EMS agencies come to Show Low on a quarterly basis to be trained to use the system. The representatives take back the knowledge to their teams, saving costs and time spent traveling to each partnering agency.

Finding a way to make this program sustainable beyond 2020 is a work in progress; securing reimbursement was the first step. Traditionally, when emergency services are activated, EMS services are only reimbursed if the patient is transported to a hospital. The Arizona Medicaid program has established the Treat and Refer program that allows first responders to treat a patient onsite when appropriate and bring him or her to a non-emergency facility for further care, including a mental healthcare facility or outpatient clinic. Timber Mesa is in the process of securing Treat and Refer Recognition that would allow EMS to get reimbursement for these kinds of transports.
A new law signed by the Arizona governor and effective in January 2021 will also help by expanding commercial insurance coverage for telehealth services, including asynchronous telemedicine and remote patient monitoring.
NIOREC has already discussed putting cost savings from the program toward population health management and value-based care. "The ideal situation would be for NIOREC to reinvest cost savings back into proactively managing patients," said Iannucci. For instance, funding a community paramedicine program or increasing home visits, primary care services, and other preventive programs that will ultimately reduce ER visits and help patients manage their chronic conditions.
It is a huge benefit for our ER doctors, hospitalists, and staff. But at the end of the day, it's the best thing for the patient to make their care better and get them the help that they need sooner.
Along with the potential benefits to the healthcare system, those involved ultimately see the NIOREC program in line with Summit's mission to bring healthcare closer to home for each patient. "It is a huge benefit for our ER doctors, hospitalists, and staff," said Peck. "But at the end of the day, it's the best thing for the patient to make their care better and get them the help that they need sooner."
