May 04, 2022
Bringing Mental Health Services to Rural Residents
by Allee Mead
 Accessing mental health services
can be difficult in many rural communities. One of the
most significant barriers is the lack of trained mental
health professionals practicing in rural areas. In
addition, residents often have trouble accessing the
resources that are available due to transportation
issues, affordability, and stigma.
Accessing mental health services
can be difficult in many rural communities. One of the
most significant barriers is the lack of trained mental
health professionals practicing in rural areas. In
addition, residents often have trouble accessing the
resources that are available due to transportation
issues, affordability, and stigma.
Holly Roberts, PhD, an associate professor at the University of Nebraska Medical Center (UNMC) and a licensed psychologist from rural Nebraska, said a major challenge to accessing mental healthcare is the distance rural residents have to travel to access services. While telehealth helps mitigate this challenge, broadband access across many rural areas can still present a barrier.

But rural communities have important resources that can be engaged to address mental wellness, namely social capital and creativity. Two programs — a new library initiative in Texas and an established crisis line in Georgia — are employing strategies to bring mental health services directly to the people in need by building upon existing community assets: trusted spaces and trusting relationships.
Creating Library Programs and Mobile Crisis Teams
Libraries for Health is a three-year pilot program that brings lay mental health workers into public libraries. "These workers have been trained in evidence-based techniques and will meet with patrons and, when needed, refer them to appropriate clinical care: in this case, a licensed therapist connected to the project," said Abena Asante, Senior Program Officer at the nonprofit St. David's Foundation, which is providing the funding and support for the program.
This program builds upon current library practices of providing information to patrons about community health resources, offering general wellness programs, and connecting patrons in distress to crisis services. The pilot program will use a task-sharing model that would train laypeople to identify mental health concerns among adult library patrons and provide nonclinical mental health supports and practices in the library space.
Providing these types of supportive interactions in spaces where community members naturally gather can help overcome barriers like transportation and stigma around mental health. The program also aims to proactively offer support to those patrons experiencing stress and anxiety so that perhaps they may not need clinical care.
To design the program, St. David's Foundation studied what libraries across the country were already doing to address mental health needs and talked to other funders that specifically work with rural libraries, the Texas State Library and Archives Commission, the Texas Library Association, and local mental health agencies and nonprofits.
Partnering closely with the nonprofit research organization RAND Corporation, Libraries for Health will take place in eight public libraries (15 branches) in and around Austin. These locations are in communities with persistent disparities that can contribute to poor mental health. Two of the participating libraries are in the rural locations of Elgin and Smithville in Bastrop County.
In Georgia, a statewide crisis line sends mobile crisis teams to people with urgent mental health issues. Teams consist of a physician and certified peer specialists: individuals in recovery who can help others access and navigate services. Responders go out in pairs or teams so there is never just one individual walking into a situation.
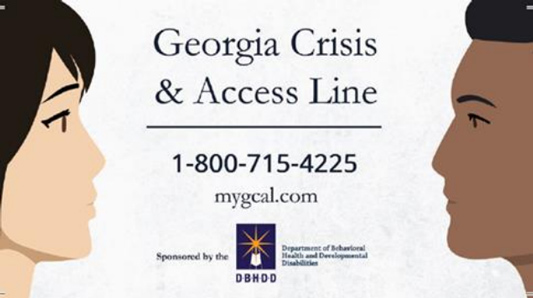
Georgia Crisis and Access Line (GCAL) is the hub that answers phone calls from across the state and dispatches the mobile crisis teams and any other needed services like emergency medical services or law enforcement.

The GCAL team also triages calls. Jennifer Dunn, Regional Services Administrator at the Georgia Department of Behavioral Health and Developmental Disabilities, gave this example: If the crisis line receives three calls — one from a jail, one from an emergency department, and someone calling from the side of the road — the GCAL team would prioritize the call from the side of the road first, since the other two locations are staffed, but all three sites would be visited by the mobile crisis team.
"We do have a 60-minute response time," Dunn said. "They have worked really, really hard to do that. And they've had to put in some extra teams at their own expense to try to make that work." She added that they let people know if a team has to answer another call first, as in the triage example above, "so nobody has to sit around and wonder." Her service area has one mobile crisis team broken into four zones.
We do have a 60-minute response time. They have worked really, really hard to do that. And they've had to put in some extra teams at their own expense to try to make that work.
When Dunn started her current position in 2007, she said there were some mobile crisis teams in the state, but they weren't available in every county and there hadn't been any mobile crisis teams in her 24-county service area in the southwest part of the state. Her department started expanding the mobile crisis teams and in 2013 had a statewide contract for these teams.
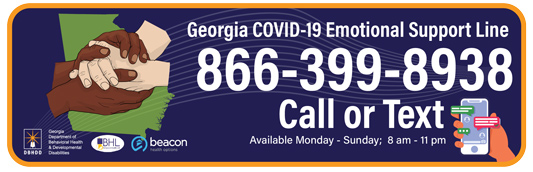
MyGCAL App and Georgia COVID-19 Emotional Support Line
The crisis line has an app called MyGCAL. Anyone who does not want to or cannot communicate verbally can use the text or chat option in the app.
The department also offers another service called the Georgia COVID-19 Emotional Support Line. It was originally intended for public health nurses dealing with stress and burnout. "But then we realized very quickly that anybody could benefit from it," Dunn said.
The Georgia COVID-19 Emotional Support Line is staffed 8:00 a.m. to 11:00 p.m. People who call this number but need more urgent services are transferred to GCAL, which can then send out a mobile crisis team.
Dunn remembers a success story from December 2021. An
individual was about to take their life when they saw an
ad for the lifeline. The individual called, GCAL sent the
mobile crisis team to their house, and that individual is
still alive today.
In another instance, the GCAL line had received a call from two teenagers. When the mobile crisis team called back, the family said that the teenagers were asleep. The crisis team insisted on checking for themselves. The teens had taken some type of substance; one teen started to have a seizure and the other one started foaming at the mouth. The two were flown to the nearest large hospital and were saved.
Addressing Rural Challenges and Need for Services
While the mobile teams are able to reach people in crisis, it can be a struggle to get those people to the services they need. One challenge in Dunn's service area is the lack of state-funded inpatient mental healthcare for children. There are some private facilities, Dunn said, but that doesn't help children whose families have low income or no health insurance. In addition, some foster children in more urban parts of Georgia are placed in more rural areas, so these children have trouble accessing any higher-level healthcare they need.
The program also recognizes that, along with access to direct provider care, access to food and shelter can influence behavioral health conditions. "In the 24 counties, I could only count two or three women's shelters; one male homeless shelter; no female homeless shelters; and three food banks, possibly four," Dunn said. Even with the services that are available, people may not have reliable transportation to get to these shelters or food banks. People with chronic mental health and other health issues also struggle to find what they need: "Right now it's very, very difficult to find a place that will take someone with chronic mental health issues that also needs dialysis," Dunn said.
Another specifically rural challenge comes when a mobile crisis team might need to call in law enforcement in a community or county with only one or two deputies on hand: "If we have to have them transport someone to a crisis center or an emergency receiving facility, it takes that deputy off the road quite a few hours," Dunn said. "And it leaves the county in a lurch because that's one less personnel that the sheriff has on hand."
The Smithville and Elgin library staff in Texas can attest to rural areas' high demand for services as well as barriers to accessing them. One of Smithville Public Library's partners, the Smithville Community Clinic, shared data from patient surveys that indicated a need for mental health services in the community. The COVID-19 pandemic also increased feelings of isolation and anxiety. "And some of that, I think, is amplified even more by the fact that we're a rural community and… the further you get away from the urban areas, the further you get away from Austin, the fewer the resources seem to become," said Judy Bergeron, Director of the Smithville library.


The Elgin Public Library's service population is about 45% Hispanic or Latino residents, according to its interim director, Paula Waak. This population is one of the reasons Elgin was interested in the Libraries for Health funding opportunity. Language can be a barrier to accessing mental health resources when people can't find a mental health professional or even written materials using their native tongue. Elgin Public Library's own staff has two bilingual staff members, who help the library better serve its patrons and answer their questions.

Another reason behind the Elgin library's participation in the Libraries for Health initiative was a community meeting to discuss what resources were currently available for suicide prevention and what other resources or programs could be implemented to provide mental health supports. Amy Miller, Community Services Director for the City of Elgin, had attended that meeting and said that "it was beyond standing room only." While the school district has suicide prevention programming, the library wanted to have its own programs to reach people outside the school district.
Staffing the Programs and Training the Employees
In the Libraries for Health initiative, the libraries will receive assistance from the RAND Corporation with hiring and training the lay mental health workers and the clinician to whom the lay workers will refer patrons. The RAND Corporation will also help the libraries with implementation and evaluation and work with them to learn more about their service population (for example, if they have high numbers of seniors, young parents, or Spanish-speaking residents) so they can design the program to better fit a community's specific needs.
The initiative also has a learning collaborative for library and mental health staff to receive training provided by RAND. The mental health staff will teach mental health activities to the library staff and in turn learn from the library staff.
Asante from St. David's Foundation discussed how libraries can use her organization's funding: "The libraries have the flexibility to use the funding to enhance their collections, to integrate mental wellness within existing programs, and to use it to buy small equipment that is going to enhance them doing the mental wellness initiative." The libraries can also use the funds to compensate the library workers participating in the learning collaborative and other related activities.
Both the Libraries for Health and the mobile crisis program in Georgia use a combination of trained laypeople and clinicians but hiring behavioral health professionals is always a challenge in rural areas. Roberts from UNMC said that rural America needs general behavioral health professionals as well as those specialized in areas such as substance use disorder and depression. Part of her work at UNMC is training future behavioral health workforce. In addition, UNMC provides technical assistance via the Mid-America Mental Health Technology Transfer Center to providers starting a new clinic.
However, new providers may not be the best fit for a program like Georgia's mobile crisis teams. In staffing these teams, Dunn recommends having "really, really strong supervision and the most seasoned clinicians" for the situations that are or might become unpredictable. She added that the clinicians answering the GCAL phone calls should be experienced as well, since they're determining how best to address a caller's needs.
"Our greatest challenge," Dunn said, "is that we have limited numbers of clinicians and personnel." She said that her department's region has had to hire people from outside the 24-county service area, which means that these people might not know the local resources as well. She added that her department has also seen an increase in crisis cases in areas when small hospitals have closed.
Knowing the Community

For other areas looking to implement a similar crisis line and mobile teams, Dunn recommends being "very, very well versed in [your] particular community. Know your stakeholders, know who they are, know who is the ER director, know who is the jail administrator, know the local sheriff, know your legislators." Another important stakeholder for this kind of program is the outpatient clinics and services.
Asante from St. David's Foundation offers similar advice to fellow funders: "Know the community very well…and test your ideas to find out if this is of interest, whether the libraries have the capacity, and whether this is something that could be promising and address some of the gaps in the community." The pilot program also has an advisory board made of library experts to gather feedback and guidance.
Know the community very well…and test your ideas to find out if this is of interest…and whether this is something that could be promising and address some of the gaps in the community.
For over a year before the launch of Libraries for Health, St. David's Foundation gathered data by conducting interviews and doing landscape analysis (determining a community's strengths and needs) with libraries and other stakeholders in central Texas. "What was interesting was that the libraries asked for us to share the information with them because they were interested in what the data revealed," Asante said.
Building Trust and Relationships
Before the Smithville library learned about the Libraries for Health initiative, the library was already involved in a mental health/COVID response grant from St. David's Foundation. This grant funded a program called Hope and Healing through Reading, "a series of book clubs for [people] who felt isolated by the pandemic and the closures and the lockdown," Bergeron said.
The book clubs took place over videoconferencing when it was unsafe to attend in person and later had a hybrid format with in-person and video options. Each club had in attendance a mental health professional, advocate, or lay mental health worker who would talk with the participants and share resources. This person held a "mental health minute" to provide brief mental health tips or exercises and ask the attendees if there were topics in the book that they want to discuss or learn more about.
Roberts from UNMC discussed how libraries and mobile crisis teams create more "access points" for mental healthcare. Increasing access points in communities, which can also include schools and primary care settings, "increases high-frequency community settings…with individuals that people trust and in a place that they trust or that is familiar to them," Roberts said. Creating additional community-based access points also takes some of the pressure off of "a primary care provider who may be the primary gatekeeper for mental healthcare in a rural community," she added.
The Georgia program also builds trust with its clients as well as its community partners. A specifically rural strength of the program, Dunn said, is that "we tend to know our clients and these friendly faces [super-utilizers of mental and other health services]. And, many times, we know their histories. A lot of the staff that work on the mobile crisis teams have worked for providers or an ER or even law enforcement before. And not only do they know some of the clients, but they know the community really well. They have the relationships. They know who the probate judge is. They know the sheriff; the sheriff knows them."
In a lot of more urban or larger areas, people don't know each other or don't know they can call each other and ask for those kinds of assistance.
For example, in December 2021, there was a day when the mobile crisis team "was just inundated with calls," Dunn said. GCAL connected with a community provider, who was able to help stabilize a situation at the local emergency department while the mobile crisis team was responding to another call. "In a lot of more urban or larger areas," Dunn said, "people don't know each other or don't know they can call each other and ask for those kinds of assistance."
"This is our community," Dunn said. "We live here, so we have a vested interest in making sure that it is successful and that people get the treatment and services that they need."
Mental Health and Suicide Prevention Resources
The 988 Suicide and Crisis Lifeline (formerly the National Suicide Prevention Lifeline), a national network of crisis centers, is available 24/7 to help people experiencing suicidal thoughts and emotional distress. The three-digit dialing code, 988, is available nationwide as of July 16, 2022.
RHIhub offers a Mental Health topic guide, Mental Health Toolkit, and Suicide Prevention Toolkit to help rural communities start, evaluate, and sustain their own programs.

