Oct 23, 2019
NIH National Center for Advancing Translational Sciences: Involving Rural America in Research
Related Article
Translational
Science: Research with Results that Touch Rural
Populations
 Getting the diagnosis of an
extremely rare condition. Hearing the terrifying news of
a cancer diagnosis. Learning for the first time that the
ongoing treatment for a chronic disease will no longer
keep that condition stable. Though these situations
differ, in those moments patients and families will ask
their healthcare providers the same question: Is there
any new research or science that can help us?
Getting the diagnosis of an
extremely rare condition. Hearing the terrifying news of
a cancer diagnosis. Learning for the first time that the
ongoing treatment for a chronic disease will no longer
keep that condition stable. Though these situations
differ, in those moments patients and families will ask
their healthcare providers the same question: Is there
any new research or science that can help us?
And if those patients and families live in rural America, the question may be different: Is there any new research or science that can help us out here where we live?
Of course, linked to both diagnosis and location, there may be a specific answer to that question. But big picture? Researchers under the umbrella of the National Institutes of Health (NIH) National Center for Advancing Translational Sciences (NCATS) are some of the teams that specifically focus on that need: getting new science to patients with illness no matter where they live. Using the principles of translational science, these researchers are bringing new drugs, new technologies, new treatments, and new cures to patients everywhere — including rural America — as fast and as safely as possible.
Dr. Michael Kurilla, director of the NCATS Division of Clinical Innovation explained the agency's goal.
"What we're doing is taking all the wonderful science that NIH is responsible for creating and turning that science into better health for people," he said. "Remember how scientists were portrayed as working in a basement, burning midnight oil, making a discovery, saying 'Eureka!'? Decades ago, if that discovery was a new antibiotic, for example, a company would come in, but only years later would a new drug go on the market. Meanwhile, the scientist went back to the basement. Now we have the academic community really taking a greater role in not just creating the science, but efficiently translating it to practical interventions and getting those interventions to healthcare providers so they can help their patients."
NCATS Goal: Translating Scientific Medical Discoveries
The NCATS translational science mission is centered in the three "D's": Develop science, demonstrate science, and disseminate science. It perhaps best resembles a systems approach where all steps – from discovering new health science to patients benefiting from that science – are interactive.
Sometimes new science needs to be vetted through an expert panel of a few patients before it goes through the process steps making it useable for all patients. At other times, it's early experimental results that need a collaborating science team to refine those results. The hallmark of translational science is that vetting new discoveries moves in many directions rather than in a single direction, an approach to ensure that new science doesn't sit on a shelf or live only in the pages of a journal, but instead becomes available to the nation's urban and rural citizens.
Learn more not only about NCATS and translational science discoveries from Dr. Kurilla, but about research that includes rural populations completed by a New York neurologist in Translational Science: Research with Results that Touch Rural Populations.
Research with Rural Community Engagement: A CTSA Program Priority
The NCATS is a federal agency that is broad and deep. Its strategic plan includes both doing and supporting scientific research. For example, its grant-making activities support research through the Clinical Translational Science Award (CTSA) Program. Some fifty-plus CTSA grantees are located across the country and are usually based in urban medical research institutions, referred to as "hubs." The hubs differ from one another just as rural regions differ one from another.
Several hubs have past and current research projects in rural areas, often the result of intentional outreach by each hub's Community Engagement (CE) program. These engagement efforts also differ between CTSA hubs. One hub's efforts might focus directly on collaboration with individual members of rural communities, while another's includes specific research partnerships with rural healthcare organizations. Yet another's effort melds their hub's CE with that of another federal agency present in the vast majority of rural communities. With examples of these CE efforts, notable is the same end goal: impacting rural America's health disparities.
Improving Public Health: Community Engagement
The Centers for Disease Control and Prevention has defined CE as "the process of working collaboratively with and through groups of people affiliated by geographic proximity, special interest, or similar situations to address issues affecting the well-being of those people." In its 2011 publication, Principles of Community Engagement, a CTSA task force highlighted that "involving the community and collaborating with its members are cornerstones of efforts to improve public health."
Arkansas's Translational Research Institute: Rural Citizens Directly Touching Research
The University of Arkansas for Medical Sciences (UAMS) is home to the Translational Research Institute (TRI). In a 2018 paper, university-based and TRI researchers shared results from the state's 2015 Behavioral Risk Factor Surveillance System (BRFSS) survey which included questions regarding research participation. (Table 1.) Noting that 42 percent of respondents were rural, many respondents indicated they'd had a research opportunity. This finding was strikingly different from previous research results. The investigators suggested that the findings could have been influenced by its broad-reaching community-based participatory research capacity. An additional finding was that nearly 48 percent of rural respondents indicated they'd be willing to participate in research.
| Table 1. 2015 Arkansas Behavioral Risk Factor Surveillance System Research Participation Survey Results | ||
| Rural | Urban | |
| Previous participation in research | ||
| Yes | 8.5 | 9.9 |
| No | 91.5 | 90.1 |
| Opportunity to participate in research | ||
| Yes | 6.8 | 8.5 |
| No | 93.2 | 91.5 |
| Willingness to participate in research | ||
| Yes | 47.8 | 44.7 |
| No | 32.4 | 31.3 |
| Undecided | 19.8 | 24.0 |
| (Total N=4,441; 42.2% rural) | ||
Source: 2018 article in the journal Clinical and Translational Science
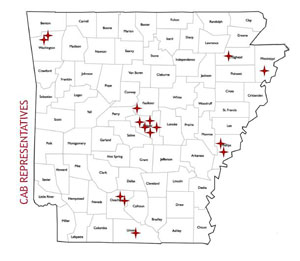
Nicola Spencer is a program manager for TRI's Community Engagement program. Spencer said the program has several rural efforts with two specifically including rural communities: the Community Review Boards (CRB) — modeled after Vanderbilt University's approach — and the Community Advisory Board (TRI CAB).
The CRB is a one-time two hour meeting in a targeted community that offers researchers an audience with community members. The community members provide feedback on aspects of the research project that range from the research question to recruitment strategies to project dissemination.
The TRI CAB also consists of community members from across Arkansas. Its purpose includes prioritizing research initiatives, increasing TRI's visibility at the community level, and facilitating community influence in research.
"One of the TRI's top priorities is the focus on rural communities which makes our CTSA different from many across the U.S.," Spencer said. "The inclusion of community members in all stages of the research process underscores the institute's goal of bringing research opportunities to the people. In order to do this well, investigators should have the opportunity to have an audience with the community members who are being affected by health disparities."

Spencer said both the CRBs and TRI CAB are well established programs, affording the CE team the opportunity to take their community-based outreach even further with a new project currently in the development phase.
"We're starting a program, the Community Partners Educated as Arkansas Research Leaders, referred to as CPEARL, that is a one year intensive training program to provide leadership training and research mentors to community leaders," she said, adding that it is the initial phase of a larger program geared to sustainable partnered research at UAMS.
Spencer said that in order to have statewide representatives from many different communities, rural and urban alike, the team has developed longstanding relationships with community leaders, non-profit organizations, and with rural health organizations, including the Tri County Rural Health Network and the Arkansas Community Health Worker Association.
TRI's Community Review Board in Action: Plain Language Prep and Lived Experience Feedback
To utilize community experts, Spencer said an investigator connects with the CE team for assistance in getting their research presentation CRB-ready with plain language and appropriate visual aids. During that prep interval, the team also begins their community outreach. With a goal of having around 8 community experts with lived experience aligning with the researcher's topic, rural participants are often needed to participate on the CRB. On the designated presentation day, the CRB members provide feedback on the research question and design. Later, the researcher receives a summary report providing documentation to help with their funding application and changes to their project. To date, the CE team has conducted 38 community review boards that included 290 community participants.
University of Washington's CTSA Hub: Institute of Translational Health Science

Designated by the acronym WWAMI because activities include sites not only in Washington, but also Wyoming, Alaska, Montana and Idaho, the University of Washington (UW) has well-established programs with a rural healthcare focus. The WWAMI medical education program aims to put physicians in the rural areas of the region. The WWAMI Rural Health Research Center often does research with a health policy focus on rural healthcare workforce and access to care. To ensure the region's rural and urban patient populations had access to clinical research opportunities, the WWAMI region Practice and Research Network (WPRN) was created in 2011. It currently includes Critical Access Hospitals (CAHs) with their affiliated primary care clinics, including Rural Health Clinics (RHCs), and Federally Qualified Health Centers (FQHCs) in addition to other types of primary healthcare systems. Thirty-two of the current 84 network clinics are in rural areas.
Of no surprise, then, is when UW's CTSA hub, the Institute of Translational Health Sciences (ITHS) does rural research, it builds on these established WWAMI rural regional relationships. The ITHS CE program's strong relationships with its WPRN clinics serve as a base from which the program also connects with other small and rural healthcare organizations throughout the five state region. Three faculty members from the university's School of Medicine (UWSoM) shared how the ITHS and the CE program work with rural community-based practices and the WWAMI region practices. They said the program also collaborates with other teams at the UW, investigators at Fred Hutchinson Cancer Research Center and Seattle Children's Hospital, and other researchers from academic institutions throughout the country.

Family medicine physician, UWSoM associate professor, and clinical investigator Dr. Allison Cole, current co-director of the ITHS CE program, said that for translational research addressing rural health disparities to be effective, it must include rural partners and good communication between the hub and rural sites.
"Research is sometimes thought of as unidirectional in that it moves from the research lab bench to the bedside to healthcare practice to eventually impact health outcomes," she said. "But translational research includes a bidirectional information flow — between practice sites and investigators — which not only allows us to build an evidence base around specific needs, it allows us to disseminate that evidence more easily. In the end, that research can make a huge impact on rural public health."

Dr. Laura-Mae Baldwin, UWSoM professor, family medicine provider, clinical researcher, and immediate past director of the ITHS CE program, further explained rural nuances for clinical investigators.
"Rural areas have distinct features and unique environments that are important to consider when translating evidence into action," she said. "Having a deep understanding of the rural context is critical in really helping to improve the health of those populations. From the clinical work they do, rural providers bring expertise to the research and from being involved in that research, bring value to their communities. I think that's so important. Research can be more effective when rural communities bring their perspectives into research teams."
Examples of ITHS Rural Research Efforts
Specific rural research projects include Cole's work using a bidirectional research approach for building rural capacity for colorectal cancer screening. Baldwin, too, used a similar approach to help a collaborative research team create the Six Building Blocks program, an evidence-based roadmap to guide rural clinics and health care organizations in redesigning opioid management processes to improve care.
"We know it's a challenge for family physicians trying to provide evidence-based care for their patients on long term opioid therapy," Baldwin said. "You'll look at the guidelines and they can give hard and fast rules. But patient care doesn't actually work that way. The process must be more patient-centered. We're still learning how to manage opioid prescribing artfully and within the limits of the evidence."
A Key to Rural Research and Quality Improvement: Data QUEST
Any practice change or quality improvement activity usually starts with data collection and ends with data analysis. But for rural healthcare organizations, an electronic health record (EHR) functionality that can accomplish this is often absent, limited, or still highly-dependent on human effort. Data-sharing barriers make it difficult for willing rural healthcare organizations to participate in research, no matter how great their interest in doing so. As part of an early demonstration project within their initial CTSA grant, the ITHS proposed creating an "electronic health data-sharing architecture" to deal with this challenge. The result? The highly successful Data QUEST.

Rural Washington and Idaho research partners sharing data through Data QUEST currently number 10 of the total 22 primary care clinic partners. Dr. Kari Stephens, UWSoM associate professor, director of Clinical Research Informatics for Family Medicine, practicing psychologist, clinical researcher, and informaticist, leads Data QUEST and developed it in deep partnership with the WPRN. She explained how it allows smaller healthcare organizations to participate in research.
"It was crucial to not put any increased demands on the rural clinical partners," Stephens said. "When we went out into communities and did feasibility studies, we specifically looked at EHR capacity and what we eventually created was this tool that allows us to reach in with a light touch and extract data for analysis. This light touch is absolutely crucial in order to not tax the smaller organizations. Usually the final data-sharing agreement with the partner gives us a read-only log-in for our technical crew and that works well."
More Details On Data Sharing
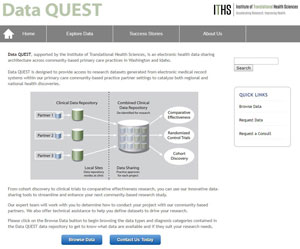
Stephens provided more detail to the steps used to engage both rural practice partners and academic investigators in research projects.
For interested rural partners, the ITHS team does a site visit with an organization's leadership to explore a value proposition and better understand their research interest. The second step is a review of the electronic health record system architecture and its ability to share data.
For academic researchers who are in planning stages of projects, the Data QUEST website allows a preview of available data elements. If this information meets their data needs, the researchers can connect with the ITHS CE team who can also offer additional how-to assistance on engaging a rural site in a project. Further helping them to explain their research protocol, ITHS can provide a one- or two-page how-to template along with research flow diagrams or other types of customized advice.
Florida's Translational Health Science Teams and USDA's Extension Collaboration

When Dr. Michael Gutter became the associate dean for Extension at the University of Florida Institute of Food and Agricultural Sciences (UF/IFAS), he found himself in conversations with the director of the university's Clinical and Translational Science Institute (CTSI) along with other university health science leaders. He said these conversations brought about the realization that collaborative research opportunities with these departments could better help UF/IFAS Extension to impact Florida's rural health disparities, a goal long part of its work.
"We realized that there were lots of great projects being done by great people and that Extension had many points of natural integration with projects happening in health sciences," Gutter said. "Extension was already in rural areas with lots of social capital and community engagement, so there was a huge potential to collaborate. Though we in Extension have different expertise than the health sciences, we're pursuing the same goals. When you put all of us in the same room together, innovation happens. Pooling talent has powerful outcomes."
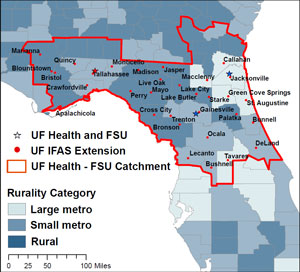
Gutter shared examples of where UF/IFAS Extension is finding itself 'getting and giving' in these health science collaborations. One natural integration point for Florida teams has been collaborating with HealthStreet, one of CTSI's CE programs. Researchers and UF/IFAS Extension workers can interact with this program that uses the expertise of Community Health Workers (CHW) in rural Florida counties that surround the CTSI and its CTSA hub partner, Florida State University. In total, CHW outreach is extending to more than 50 counties across the state.
Ideas for Partnering with Extension
Gutter suggested a few Extension community engagement activities that might assist health science investigators and rural healthcare organizations in their population health work:
- Connect with county Extension Advisory Boards, some which even include rural local healthcare providers.
- Take advantage of Extension's County Needs Assessment evaluations which may overlap or add to information from a healthcare organization's own assessment.
- Review Extension's educational program activities and outreach work for collaborative opportunities or to adopt some of Extension's evidence-based models, like Dining with Diabetes.
Another project, UF CTSI's Our
Community, Our Health, uses a livestream Town
Hall meeting framework and presentations are archived for
public access. For example, one
past event moderated by a CTSI advisory board
member covered opioid misuse. How is Extension
connecting in this setting? Gutter said events like
these provide Extension teams on campus and out in
the field with formal "listening session"
opportunities that, in turn, lead to more collaborative
ideas and opportunities that help spur the scholarly work
that is also an integral part of Extension.
"At UF, everyone seems to be considering partnership possibilities or at least asking the question, 'Can we work with Extension?'" Gutter said. "We don't always arrive at a perfect yes or a perfect no, but there's often a 'yeah, we can figure that out.' This works because then we're all on a path forward to dealing with rural health disparities."
University of Florida's National Un-Meeting
Gutter had frequent conversations with the CTSI's director, Dr. David Nelson, about how well their collaboration was working.
"We couldn't get over the fact that what we were doing here with Extension and health science research collaboration was working so well, yet didn't seem to be happening in other places," Gutter said. "We felt that what was happening here in Florida was too important to not share with other CTSA hubs around the country and we decided to host the Un-Meeting."
The Un-Meeting, a national event held in April with support from the coordinating center for the national CTSA Program, brought around 120 Extension and health science experts together to explore untapped areas of collaboration. Representing nearly 30 states, Gutter said attendees seemed to more clearly understand that rural communities are unique from one another and much less homogenous than urban areas. Additionally, he said the meeting helped raise awareness that Extension is a potential research partner in almost every county in the country and possesses the social capital to help promote community engagement that's so important to translational science work.
An Un-Meeting differs from a traditional conference format in that it allows attendees to create somewhat of a real-time agenda by using small group interactivity and conversations around a common theme.
In the End: It's About Turning Science into Health
The CTSAs in Arkansas, Washington, and Florida are just three of many translational science centers that use rural community engagement to conduct research addressing health disparities. NCATS's Clinical Innovation director Kurilla said since including rural areas has been a focus from the agency's origins, there is now a fairly large body of translational science work impacting those populations.
"There are many who look at the NIH and recognize it as an agency largely concerned with scientific discoveries and journal publications," he said. "I think people may be surprised that it's also focused on the downstream translation of that science directly into health. We are very focused on the later stages of a scientific discovery and our job is turning that science into health. Particularly for those of us at NCATS, that includes that last mile where we are meeting the patient."

