Sep 01, 2021
Keeping the Doors Open: Vulnerable Rural Hospitals Benefit from Federally Funded Technical Assistance
 The rural
hospital's list of challenges is familiar. Detailed in
the
American Hospital Association's 2019 Rural Report,
persistent challenges for rural hospitals include ongoing
healthcare workforce recruiting and retention issues
associated with caring for an older, sicker, and poorer
population. Experts elevated another challenge: the rural
hospital closure crisis.
The rural
hospital's list of challenges is familiar. Detailed in
the
American Hospital Association's 2019 Rural Report,
persistent challenges for rural hospitals include ongoing
healthcare workforce recruiting and retention issues
associated with caring for an older, sicker, and poorer
population. Experts elevated another challenge: the rural
hospital closure crisis.
Though experts also point out that rural hospital closures have a very negative impact on a community's economics, a 2019 report demonstrated that closures negatively impact a community's mortality. With rural hospitals representing more than half the hospitals in the U.S., the Federal Office of Rural Health Policy provides multiple programs to meet the unique needs of rural hospitals, like the new Vulnerable Rural Hospital Assistance Program (VRHAP) that provides technical assistance to hospitals at risk for closure. Operated by the Texas A&M Center for Optimizing Rural Health (CORH), 174 hospitals have received technical assistance since its 2019 start.

Principal investigator Dr. Nancy Dickey, along with the program's director of technical assistance, Dr. Bree Watzak, and project director, Andrea Brewer, discussed the program's offerings. According to Watzak, their organization was well-positioned for the cooperative agreement award because of the work done in their home state of Texas.
"Our state has had the most rural hospital closures," she said. "From our work here in Texas, we'd developed a technical assistance approach that focuses on leadership, community engagement, and hospital operations. Specifically, for this work, we developed a scoring rubric to select 30 participants per year. Five of the most at-risk hospitals receive additional assistance, including onsite visits."
- Health of Community (15 points)
- Community/Facility Level of Readiness to Participate (20 points)
- Level of Vulnerability (50 points)
- The Financial Distress Index calculated by the University of North Carolina Sheps Center
- Quality/Experience
- Operations
- Finance (previous fiscal year)
- Distance from the applicant community to next nearest hospital (15 points)
An Oklahoma Participant Perspective
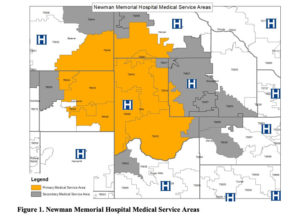
Financial controller Brittany Rash, an active VRHAP program participant from Newman Memorial Hospital in Shattuck, Oklahoma, explained that for her organization, the VRHAP program's positive impact has been so broad and deep, they are actually now applying for their fourth consecutive year.

"When I first came to Newman, I had little experience with Critical Access Hospital finances," Rash said. "I'd gotten an email providing information about the opportunity from our State Office of Rural Health. Looking at the program application, I thought, gee, this application is so straight forward, it doesn't seem to require the usual need for four grant writers and four days. I can actually quickly apply for this myself. Without knowing what I was really getting into, I signed up. It was the best thing I ever did. And I've kept applying because it has made such a tremendous difference for our hospital."
Understanding VRHAP's Tiering Process

"Tiering is part of the rubric," CORH's project director Brewer noted. "The application outlines the scoring, which includes a review of an organization's financial status. We do work with North Carolina Sheps Center who calculates an applicant's Financial Distress Index. That's an important measure of a hospital's vulnerability and carries the most weight."
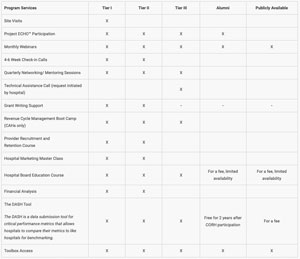
The CORH team said they offer fourteen services, and access to these services differs according to the organization's tier assignment. All three tiers receive remote technical assistance. The five most vulnerable hospitals are stratified as Tier I and receive onsite CORH team visits. Tier I and II hospitals are able to access classes such as provider recruitment and retention and hospital marketing.
Tier I Onsite CORH Team Visits

Dickey explained that CORH's Tier I participant onsite visits are designed to engage hospital leadership — including board members — as well as community voices that often go unheard in traditional health needs assessments. She said that these personal face-to-face interactions have emerged as "a very powerful tool."
"Though COVID did put limitations around onsite visits, we will tell you that from those visits that did happen, not only did we come away with deeper insights around the organization and their community, but we developed important relationships," Dickey said, explaining that site visits occur at cohort year start and completion. "Because of COVID, we may never have enough information to fully analyze the benefits of that relationship building. But I'd be willing to bet that if we continue to do this beyond year five, data will show that the organizations that get site visits had a measurably higher level of positive outcomes than those who only got to know us virtually. It just is what it is. Onsite visits are proving incredibly valuable."
Tier II and III Benefits
Brewer pointed out that although the majority of applicants seem hopeful for the Tier I designation, stories from Tier II and Tier III cohort members demonstrate that CORH's assistance benefits the other selected participants. One such example is Oklahoma's Newman Memorial. Brewer noted that Newman applied for three consecutive years and was accepted as a Tier II hospital for the first two years and as a Tier III hospital for the 2020-2021 cycle. Rash shared more about her organization's successes.
"We've been able to implement changes and add services," Rash said, referring to two specific priorities addressed by webinars and Project ECHO® participation.
"First, I knew that our charge master was nowhere close to where it needed to be," she said. "It is a beast to tackle, even if you have the knowledge. My second priority was the cost report. As a Critical Access Hospital, your cost report is everything. If you're not utilizing it to its highest capacity, you might as well shut the doors."
Rash said in addition to the charge master and cost report changes, technical assistance around adding healthcare service lines has not only brought increased revenues but brought new community awareness to the hospital. Again, she cited two specific examples.
"One presentation was geared to growing a swing bed program," she said. "It was always a service we offered, but it was an underutilized service. The VRHAP presentation information stressed that because we're a rural community, we might need to keep our patients longer because home resources after discharge aren't as available as they are in urban areas. We knew our hospital nurses were saying, 'This patient can go home.' Yes, they could — if they could live there at home in a hospital bed. The reality was that until a patient can go home and live a safe lifestyle at home, they are not ready to go home. The program's information showed that being able to take those patients through a few more clinical steps and then linking that clinical improvement to a few swing bed days, patients benefited and we had more cash to operate. That information put everybody in the hospital on the same page."
A second example was infusion services — services that she said led to more cars in the hospital parking lot — pointing out that nothing squelches a rumor that a rural hospital is about to close like a full parking lot. Additionally, she noted that having infusion services has increased appreciation of the hospital's service lines.
"Prior to offering outpatient infusions, people were having to take off days from work or students would have to miss school along with their parents missing work," Rash said. "Driving three hours to Oklahoma City just to get a two- or three-hour infusion exhausts everyone. Physically and financially. Our community seems very appreciative that we can now offer that in our hometown. It's been so important that we're now really working hard to find a way to offer chemotherapy infusions."
Rash also shared that all of the results from VRHAP's technical assistance converged in one single important spot: the hospital's financial bottom line.
"We've been able to grow our net revenues by almost $500,000 each year I've participated," Rash said, reiterating that applying for the VRHAP program was the best thing she ever did.
So Much VRHAP Information: Disseminating the Assistance
Dickey also acknowledged that the program's offerings are so extensive that, in some cases, a team approach to the VRHAP curriculum may be beneficial.
 "As we review
the most successful participants, we've found a
pattern," Dickey said. "An organization seems to gain
more from our assistance when more representatives
participate. No single person is likely to have the
time on their schedule or perhaps the background or the
interest to participate in every activity we offer.
Some topics lend themselves to quality improvement, so
the chief nursing officer might want to be involved. In
another case, the offering might be financial and best
suited for the chief financial officer. From the first
calls we have with our new cohort members, we encourage
them to think about participating as a team."
"As we review
the most successful participants, we've found a
pattern," Dickey said. "An organization seems to gain
more from our assistance when more representatives
participate. No single person is likely to have the
time on their schedule or perhaps the background or the
interest to participate in every activity we offer.
Some topics lend themselves to quality improvement, so
the chief nursing officer might want to be involved. In
another case, the offering might be financial and best
suited for the chief financial officer. From the first
calls we have with our new cohort members, we encourage
them to think about participating as a team."
Most Popular Topics and Project Surprises
The CORH team pointed out that their most popular publicly available webinars include topics ranging from hospital board education to charge master review to tips on managing burnout, the latter especially helpful in addressing the increased burnout issues due to COVID. The most popular 2020-2021 ECHO presentations — only available to the cohort — were sessions covering swing beds, CARES Act hospital benefits, and revenue cycle management.
With the fourth-year VRHAP application deadline having passed, the CORH team reviewed not only their successes but their surprises. Watzak shared a surprise associated with the ECHO presentations.
"Attendees would begin chatting with each other, privately, not to the whole group, and making connections," Watzak said. "They'd say, 'I'm having that trouble, too. Can I talk with you offline?' When we'd call our Tier I and II cohort four to six weeks later, they'd tell us about those participant-to-participant connections, saying 'Oh, so-and-so walked me through how to do X, Y, and Z.' They can bounce ideas off each other and connect with somebody having the same struggles. They connected outside of us and because of us. That is good. We want them to make friends and help each other."
From the onsite visits with the Tier I cohort, Dickey said that the team made several surprise discoveries: unique, quality service offerings provided by vulnerable hospitals were going unnoticed by the participant's community.
This example showcases the need for one of our most emphasized programs across the past three years of our work: a vulnerable hospital needs to have a communication and marketing program.
"One specific example was an organization doing two things: something very special for newborns with breathing problems and the service line addition of a cardiac catherization lab," she said. "They'd even done their first cardiac cath and our team discovered that nobody in town knew about these incredible and unique services. This example showcases the need for one of our most emphasized programs across the past three years of our work: a vulnerable hospital needs to have a communication and marketing program."
"That doesn't mean you have to bring in a four-star marketing group," Dickey added, pointing out the availability of a local newspaper in most rural communities. "Every one of these services needs to be turned into a news story as opposed to an advertisement. Invite your local news organization to have a cup of coffee with you, the CEO, or you, the chief nursing officer. Consider doing that once a month, once a quarter. I practiced as a family physician in a small town for 20 years, I've experienced the power around the fact that if ten people know about something new and worthwhile, within days — if not hours — 150 people will know. It was a bit of a surprise to us to see that these Tier I organizations could be doing such a great job of addressing healthcare issues they saw as needs and doing them so very well, but their community remained totally unaware of the important things happening at the hospital."
If interested in participating in Year 5 of the VRHAP technical assistance program, the CORH team will welcome applications through their website portal beginning June 1, 2022.
Participants Get Surprised, Too
Starting with her initial surprise at the simplicity of the VRHAP application, Newman's Rash pointed out that the program was clearly respectful of the limited resources — especially time — inherent to CAHs across the country.
"I knew that every hour I spent participating in an ECHO session or listening to a webinar was going to pay off big," she said.
Rash said she's also been surprised at the depth and breadth of CORH's technical assistance as well as the tenacity the CORH team brought to problem-solving.

"If we had a group of 12, and each of us would bring an issue to the table, [the CORH team would] not stop until they'd found the subject matter expert for our concerns," Rash said. "In addition, during the monthly ECHOs, we'd present our issues and the subject matter expert provided their expert opinion. Yet, the expertise didn't stop with one-way information. At the end of their presentation, we were able to get more help. For example, 'You didn't touch on this and it's my biggest issue.' Or sometimes this would be the comment: 'You said this, but I feel like this is actually something else and I might run into a problem here. How would you handle it then?' The expertise we were offered was very important."
Rash also said that although as a cohort member she received no-cost assistance, she was not unaware of the monetary value of the subject matter expertise she received.
"With most rural hospitals, we don't have the cash flow to reach out to a lot of the experts," she said. "We just can't afford to have consultants on speed dial and there's always going to be an issue we need help with. Knowing that as part of this program we had a way to resolve our problems, having access to experts was huge. At Newman, we were a struggling hospital that was very close to shutting the doors. I understood that we did have a lot of opportunity, but we had to grow to stay open. I just tried to really maximize all of the information I was privileged to receive. I was able to use the information in so many different areas to really bring our hospital together to increase that bottom line so we could continue to serve our community. We got busier. It just came together. We're still open."

