Oral Health in Rural Communities
The regular preventive care of the teeth and gums is important in maintaining quality of life and overall health, playing a role in controlling diseases such as diabetes and heart disease. Yet, rural communities often lack adequate oral healthcare and subsequently miss out on the benefits of good oral health as well. Several factors have been well documented as contributing to the oral health challenges of rural America:
- Access to dental care – Many rural communities lack access to oral health providers due to geographic isolation and workforce maldistribution.
- Oral health literacy – A 2009 study found that health literacy is lower among rural populations. In terms of oral health, poor health literacy can result in poor oral hygiene and difficulty in navigating the oral health system. In addition, rural residents with low health literacy are more likely to consume sugar-sweetened beverages and more prone to dental caries, according to a 2016 report.
- Fluoridation of water supplies – A higher proportion of homes in rural communities are not served by community water systems and as a result cannot receive the preventive benefits of optimally fluoridated water.
- Tobacco use – Cigarette smoking is more prevalent in rural areas than in urban areas (24.1% of adults in nonmetro areas versus 15.7% of adults in large metro areas), as well as smokeless tobacco use (6.3% of adults in nonmetro areas versus 2.6% of adults in large metro areas), according to a 2024 SAMHSA report.
This guide highlights the resources that will support rural healthcare providers and others in promoting access of oral health services to rural adults and children.
Frequently Asked Questions
- What oral health disparities are present in rural America?
- What barriers do rural communities and populations face regarding oral healthcare?
- How do I start a dental health service in my local community?
- What are some innovative solutions to address oral health in rural communities?
- Do rural areas have sufficient dental health workforce?
- What are dental therapists and how do they provide access to care for rural populations?
- Where can I find information about fluoridation of rural community water supplies?
- Who can I contact for information about oral health programs in my area?
What oral health disparities are present in rural America?
Oral health disparities in rural areas are due to factors such as workforce shortages and dental health insurance coverage on top of the geographic and social factors that affect the health outcomes of rural people broadly. Some of the specific oral health disparities in rural America are:
- In 2019, 57.6% of adults age 18-64 living outside of a metropolitan statistical area (MSA) reported that they had visited the dentist in the past year, compared to 66.7% of those living within an MSA, according to Health, United States, 2020-2021.
- According to a 2021 study, rural children were more likely (7.3%) to report having teeth in fair or poor condition than urban children (6.6%) and less likely to receive fluoride treatment (46.6% versus 52.5%) and dental sealant (19.5% versus 22.5%) than urban children.
- A 2013 report shows rural counties have higher percentages of people with partial edentulism, having had several teeth extracted, when compared to urban (urban, 38.4%, high poverty rural 51.3%, other rural, 45%) and counties with high rates of full edentulism, having all teeth missing, are also rural (urban, 4.3%, high poverty rural 10.5%, other rural, 8.2%).
- Seniors in rural areas are less likely than their suburban or urban counterparts to have visited the dentist in the past year and more likely to have all their teeth removed due to decay or gum disease, according to a 2018 report.
What barriers do rural communities and populations face regarding oral healthcare?
In its 2004 report, the National Advisory Committee on Rural Health and Human Services identified several factors that contribute to the problems of accessing dental care in rural America that still hold true today:
- Geographic isolation – There are fewer dental health professionals in rural areas resulting in people having to travel farther to obtain oral healthcare.
- Lack of adequate transportation – Public transportation systems are often nonexistent, causing rural residents, particularly low-income residents, difficulty in traveling to a dentist.
- Rate of poverty is higher in nonmetro areas – Rural populations living in poverty often cannot afford dental healthcare or purchase dental health insurance.
- Large older adult population – Rural America has a higher percentage of people age 65 and over, who are less likely to have dental coverage, as they generally are not employed, and Medicare does not provide dental benefits.
- Difficulty finding providers willing to treat Medicaid patients – Low reimbursement rates cause many dentists to not accept Medicaid or Children's Health Insurance Program (CHIP) patients. According to a 2021 report from the American Dental Association's Health Policy Institute, Medicaid only reimbursed 61.4% of the private insurance reimbursement rate on average for children and 53.3% for adults in 2020.
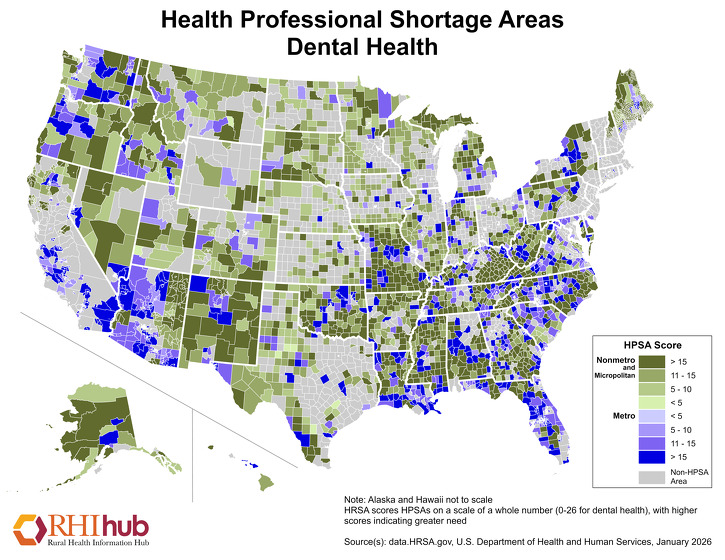
- Acute provider shortages – Approximately 66% of the nation's Dental Health Professional Shortage Areas are in rural America as of September 30, 2025. For the most current figures, see HRSA's Designated Health Professional Shortage Areas Statistics.
- Lack of dental insurance – A 2010 study found that employers in rural areas are less likely to offer dental insurance than those in more populated areas.
How do I start a dental health service in my local community?
Several resources are available that provide information on how to develop a rural dental health service:
- Funding & Opportunities by Topic: Oral Health –Includes both national and state funding programs that support projects that develop, enhance, and/or sustain dental health services in rural communities.
- The Rural Oral Health Toolkit – Designed to help a rural community implement an oral health program or service.
- Safety Net Dental Clinic Manual – Discusses aspects such as start-up costs, picking a location, construction, rules and regulations, mobile dental units, and required staffing
- Expanding the Dental Team: Increasing Access to Care in Public Settings – Provides examples of midlevel dental therapists working to provide dental care to communities with provider shortages
What are some innovative solutions to address oral health in rural communities?
The lack of access to oral healthcare due to cost, insurance coverage, and other social determinants of health in rural communities has spurred the creation of several innovative models to address this barrier. The National Rural Health Association and CareQuest Institute for Oral Health coauthored a Compendium of Rural Oral Health Best Practices which discusses oral healthcare integration into primary care, school-based oral healthcare delivery, and teledentistry as several prominent models that have been deployed effectively in rural areas.
Oral Health Integration
Oral health integration refers to the integration of basic or preventive oral healthcare into primary care settings in order to expand access to dental care for communities with dental care provider shortages. In the U.S. Department of Health and Human Services' (HHS) Oral Health Strategic Framework: 2014-2017, the integration of oral health and primary care was identified as the number one goal in combating oral health disparities. Integration of services often includes co-location of services. The model allows for improved communication and coordination between dental and primary care providers.
Some integration models and resources:
- Rural Oral Health Toolkit: Oral Health-Primary Care Integration Model – Provides an outline of the model and highlights key resources for implementing oral health integration.
- Returning the Mouth to the Body: Integrating Oral Health & Primary Care – Describes how coordinating oral health and primary care services can address dental health disparities, including in rural areas
- Integrating Oral and General Health Through Health Literacy Practices: Proceedings of a Workshop – Highlights a round-table discussion on the importance of health literacy in oral healthcare integration.
Mobile Oral Health Programs
Many successful mobile oral health programs have been developed and widely used in rural America. Mobile dental vans and other portable dental clinics have traveled to various rural population centers to provide preventive care, x-rays, and other dental procedures. The Rural Oral Health Toolkit identifies resources and best practices to help implement a rural Mobile Dental Services Model.
Teledentistry
In the aftermath of the COVID-19 pandemic, there has been an expansion of telehealth into oral healthcare. Teledentistry, like other forms of telemedicine in primary and behavioral healthcare, utilizes video and audio technology to diagnose, educate, and engage with patients remotely. According to a best practices guide from the U.S. Department of Health and Human Services, teledentistry can be used for examinations and screenings, follow-up care, emergency care, virtual examinations, and treatment planning. For additional information about increasing rural access to healthcare with telehealth, see Telehealth and Health Information Technology in Rural Healthcare.
Other Models
Rural providers have used existing healthcare technologies, practices, and methods to bring preventive oral care to their communities, such as the use of school-based health centers, telemedicine, and community health workers. Models for each are listed here, respectively:
- School-Based Health Center Dental Outreach – A consortium of 5 School-Based Health Centers worked together to improve the oral health of children in 6 rural parishes (counties) in Louisiana.
- SMILES Dental Project – A program in Colorado that uses a virtual dental home model that allows dental hygienists in rural and remote areas to provide basic preventive dental care under the supervision of a dentist via teledentistry.
See Models and Innovations: Oral health for additional model programs providing oral health services in rural locations.
Do rural areas have sufficient dental health workforce?
Rural communities often suffer from a lack of oral health providers. According to the Health Resources and Services Administration (HRSA), as of September 30, 2025, 5,185 of the nation's 7,254 Dental Health Professional Shortage Areas (HPSAs) were located in rural or partially rural areas. For the most current figures, see HRSA's Designated Health Professional Shortage Areas Statistics.
According to the HRSA Area Health Resource File, 2022-2023, there were 4.7 dentists for every 10,000 people in rural areas, whereas urban areas had 7.8 dentists per 10,000 people.
The shortage of dental professionals is frequently cited as a cause of the oral health disparities that exist in rural communities. Contributing factors to the shortage include:
- Limited slots in dental schools
- An unwillingness of providers to work in rural areas
- A large number of dentists retiring
- The growing trend of specialization in dental care
The Rural Monitor article Washington Program Trains Dental Super-Generalists to Serve Rural Communities describes a dental education program that is addressing these factors by accepting students interested in rural practice and providing specialized training to prepare them for rural practice.
Loan Repayment for Oral Health Careers
General practice dentists and registered clinical dental hygienists may qualify for the National Health Service Corps Loan Repayment Program. This is a federal program that is open to licensed dental health providers who are employed or have accepted employment at a National Health Service Corps approved site. The Indian Health Service also has a loan repayment program for those who qualify.
For more information about loan repayment programs, see our topic guide on Scholarships, Loans, and Loan Repayment for Rural Health Professions.
What are dental therapists and how do they provide access to care for rural populations?
Dental therapy is the addition of midlevel providers to the dental healthcare system. Like physician assistants in medicine, dental therapists are able to provide preventive and restorative care.
In 2009, Minnesota authorized dental therapists to practice in all of the states' underserved areas. Minnesota has three types of dental therapist programs: Oral Health Care Practitioner (OHCP) Master's degree program; Bachelor's and Master's level Dental Therapy degree; and Master's degree in Advanced Dental Therapy.
Maine (2014), Vermont (2016), Arizona (2018), Michigan (2018), Washington (2019), Nevada (2019), Idaho (2019), Montana (2019), Connecticut (2019), and New Mexico (2019) passed legislation authorizing dental therapists to practice in their states, according to a 2021 PEW report. For further information on the above programs, see:
- Working With Midlevel Providers: Dentists' Perspectives
- Dental Therapy Toolkit: A Resource for Potential Employers
- An Advanced Dental Therapist in Rural Minnesota: Jodi Hager's Case Study
Dental therapists have been able to practice on tribal lands in Alaska since 2004, in one tribal nation in Washington since 2016, and two tribes have been authorized under a state pilot project in Oregon since 2016. Alaska has been a leader in using dental therapists — called Dental Health Aide Therapists (DHATs) in that state — to meet the needs of people in very remote villages. DHATs are trained in Alaska in a two-year, post-high school competency-based primary care curriculum that incorporates preventive and clinical strategies. DHATs have been providing preventive and basic dental care since 2005. Program evaluations have shown that DHATs are technically competent and successfully treating patients under the general supervision of dentists. A 2018 study found that DHATs were linked to improved dental outcomes such as fewer extractions among children and adults in tribal communities in Alaska's Yukon-Kuskokwim Delta. Additional information about Alaska's program is available from the Alaska Native Tribal Health Consortium.
The Swinomish Indian Tribal Community, a federally recognized tribe in Washington State, has expanded their dental team to include a Dental Health Aide Therapist. Outside of Alaska, this is the first tribal community to train a student to become a Dental Health Aide Therapist.
In 2016, the Oregon Tribes Dental Health Aide Therapist Pilot Project was developed with the purpose of creating a new category of dental care providers and to provide dental therapy training to tribal members.
Where can I find information about fluoridation of rural community water supplies?
Community water fluoridation is consistently found to be one of the most effective means of preventing tooth decay. According to a 2016 article, every $1 spent on fluoridation saves $38 in treatment costs in a community with a population of 20,000+. However, it is proportionally more expensive to fluoridate small community water supplies than large ones. For communities with fewer than 5,000 people, the ratio is $6 saved to every $1 spent. In addition, most of the 12.6 percent of U.S. residents using private wells are located in rural areas. The natural fluoride level in these wells is typically too low to prevent tooth decay.
The Centers for Disease Control and Prevention (CDC) Community Water Fluoridation website has information about water fluoridation, including maps, safety guidelines, and state statistics. The CDC's My Water's Fluoride website provides information on the fluoridation status of local community water supplies. Also, Water Fluoridation and Dental Health Indicators in Rural and Urban Areas of the United States reports on the availability of fluoridated water in both rural and urban settings and compares fluoride availability to the dental health of adults and children.
Who can I contact for information about oral health programs in my area?
The Association of State and Territorial Dental Directors (ASTDD) maintains a directory of state oral health programs with contact information and a description of their programs.