Rural Emergency Hospitals (REHs)
Congress established the Rural Emergency Hospital (REH) designation in December 2020 in Section 125 of the Consolidated Appropriations Act, 2021 (Public Law 116-260) in response to the loss of essential healthcare services in rural areas due to hospital closures. The REH designation is designed to maintain access to emergency and outpatient hospital services in communities that may not be able to support or sustain a Critical Access Hospital or small rural hospital. According to the North Carolina Rural Health Research Program, 152 rural hospitals closed or stopped providing inpatient services between January 2010 and October 2025. In addition, a February 2025 Chartis Group report identified 432 financially vulnerable rural hospitals at risk of closing.
The REH designation became effective on January 1, 2023. REHs are required to provide 24-hour emergency and observation services and can elect to furnish other outpatient services. An REH cannot have inpatient beds, except those furnished in a distinct part unit licensed as a skilled nursing facility. Facilities designated as an REH receive enhanced Medicare payments for certain outpatient services and additional monthly facility payments. (see What are the benefits of REH status?)
This guide provides resources regarding the following REH-related areas:
- Payment information
- Regulations regarding REH status and operations
- Key organizations in the field
Frequently Asked Questions
- What types of facilities are eligible for REH status?
- What are the benefits of REH status?
- What are the location requirements for REH status?
- Are all the benefits of REH status available in every state?
- How many REHs are there and where are they located?
- What services are REHs required to provide?
- Are there special staffing requirements for REHs?
- Is there a limit on the length of stay for patients at REHs?
- What kinds of agreements does an REH need to have with an acute care hospital?
- Are Rural Emergency Hospitals eligible for the 340B program?
- What are the quality assurance and quality improvement options for REHs?
- What is the REH survey process?
- What sources of capital funding exist for REHs?
- Who can I contact for technical assistance and support related to Rural Emergency Hospitals?
What types of facilities are eligible for REH status?
Critical Access Hospitals and rural acute care, tribally-operated, and Indian Health Service (IHS) hospitals with 50 or fewer beds that were open on December 27, 2020, are eligible to apply for Rural Emergency Hospital (REH) status. Facilities that closed after December 27, 2020, are eligible to apply for conversion to an REH. All REHs must meet the REH Conditions of Participation. The North Carolina Rural Health Research Program provides information on hospitals that converted to REH status since January 1, 2023, in both list and map format.
How Many Hospitals Might Convert to a Rural Emergency Hospital (REH)? used data from 2019 and 2020 to estimate that 68 rural hospitals may consider becoming an REH. A December 2022 follow-up analysis, Characteristics of Rural Hospitals Eligible for Conversion to Rural Emergency Hospitals and Three Rural Hospitals Considering Conversion, noted that REH conversion may attract more hospitals than the authors initially anticipated. In both analyses, however, the researchers emphasized that their estimates were based on limited data, different selection criteria would result in different potential REH converters, and there is continued uncertainty about how many facilities will pursue REH status. A February 2023 study from the Chartis Center for Rural Health found that 389 rural hospitals may consider converting to REH status, with 77 hospitals "ideal candidates" for conversion.
What are the benefits of REH status?
Rural Emergency Hospitals receive the following benefits:
- Payment of the Outpatient Prospective Payment System (OPPS) rate plus 5% for all outpatient department services provided to Medicare patients. Laboratory services, Skilled Nursing Facility (SNF) services provided in a distinct part unit (DPU), and other services that are not considered REH services are paid under their respective fee schedules and do not receive an additional 5% payment. A November 2023 final rule enabled Indian Health Service (IHS) facilities that convert to REH status (IHS-REHs) to be paid under the All-Inclusive Rate (AIR) established by IHS for Medicare outpatient services instead of the OPPS.
- An additional monthly facility payment. According to the CMS publication Medicare Learning Network: Rural Emergency Hospitals, each REH, including IHS-REHs, received $285,625.90 per month in 2025. This additional payment will increase each year by the same percentage as the hospital market basket increase.
- Flexible staffing and services, to the extent permitted under state licensure laws.
- Access to technical assistance through the Rural Health Redesign Center's Rural Emergency Hospital Technical Assistance Center (REH-TAC).
REH status does not guarantee a better financial situation for hospitals that choose to convert. Each facility must conduct its own analysis to determine if conversion is financially advantageous and will meet the unique needs of its community. For example, Observed Factors Influencing REH Conversion Decisions: Insights from the Rural Emergency Hospital Technical Assistance Center's Financial Modeling Process notes that the loss of swing beds and 340B program revenue were among common concerns of hospitals exploring conversion to REH status.
Facilities that convert to REH status can transition back to their original Critical Access Hospital (CAH) or acute care hospital designation. However, if a CAH received its designation prior to January 1, 2006, based on state determination as a "necessary provider" of healthcare services to residents in the area, it may not be able to return to CAH status unless it meets all location requirements and Conditions of Participation. REHs are also eligible to become an approved National Health Service Corps site, which allows REHs to recruit and retain qualified clinicians.
What are the location requirements for REH status?
To be eligible for REH status, acute care hospitals must have 50 or fewer beds and either be in a rural area or had an active rural reclassification as of December 27, 2020. The Centers for Medicare & Medicaid Services (CMS) uses the Office of Management and Budget's Core Based Statistical Areas (CBSA) to identify micropolitan and noncore counties as rural counties, as outlined in section 1886(d)(2)(D) of the Social Security Act. You can use the Am I Rural? tool as a first step to see if a location’s CBSA is classified as metropolitan or rural (micropolitan or nonmetropolitan), but note that your Am I Rural? report is not a guarantee of your eligibility for the REH designation. If you have questions or want further verification of your location status, please contact your state survey agency.
Are all the benefits of REH status available in every state?
No. First, each state will need to establish licensing, staffing, and other regulatory requirements for Rural Emergency Hospitals (REHs). Because the REH is a new provider type, state governments will need to modify existing laws and regulations to accommodate the REH designation. The Health Costs, Coverage and Delivery Database, maintained by the National Conference of State Legislatures, tracks which states have proposed and enacted laws regarding REH licensure. REH-related laws can be found by searching for "Rural Emergency Hospital" in the Summary Text Search box of the database. However, some states have existing laws and regulations that can apply to REHs. If a state licenses REHs under the same licensure rules as other facilities, the REH must comply with those rules. If a state's rules are not compatible with the Medicare REH Conditions of Participation, the facility will not be able to operate as an REH. The National Academy of State Health Policy offers a guide to legislative and regulatory considerations for states interested in establishing the REH provider type.
How many REHs are there and where are they located?
The North Carolina Rural Health Research Program maintains a list of Rural Emergency Hospitals, which includes the hospital name, address, previous Medicare payment designation, and effective date of REH status. The March 2024 Medicare Payment Advisory Committee (MedPAC) Report to Congress describes the characteristics of the 21 hospitals that converted to REH status in the first year of the designation, including hospital type and Medicare payment designation before conversion, distance to nearest general acute care hospital, inpatient and outpatient visit trends, and more.
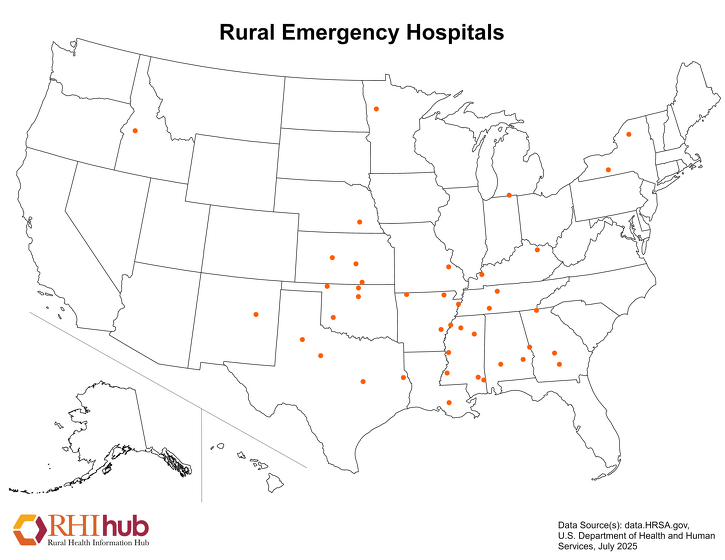
As of October 2025, there are 42 REHs located throughout the United States.
The following map shows the locations of Rural Emergency Hospitals across the United States as of July 2025. State-level healthcare facility maps are also available.
What services are REHs required to provide?
Rural Emergency Hospitals are required to provide the following services:
- 24-hour emergency services
- Laboratory services identified in the Critical Access Hospital Conditions of Participation and consistent with the needs of the patient population
- Diagnostic radiologic services
- Pharmacy or drug storage area
- Discharge planning by, or under the supervision of, a registered nurse, social worker, or other qualified professional.
In addition to these services, REHs are allowed to provide additional outpatient services, including behavioral health, radiology, laboratory, and outpatient rehabilitation. An REH may also establish a separate, distinct part unit licensed as a Skilled Nursing Facility (SNF) to provide post-REH or post-hospital services. REHs can also serve as an originating site for telehealth services.
Are there special staffing requirements for REHs?
The emergency department of an REH must be staffed 24 hours a day, 7 days a week. Like Critical Access Hospitals, a doctor of medicine (MD) or doctor of osteopathy (DO), a physician assistant, a nurse practitioner, or a clinical nurse specialist with training or expertise in emergency care must always be onsite or on-call and available onsite within 30 minutes, or within 60 minutes if certain frontier or remote area criteria are met. REHs must meet CAH Condition of Participation: Emergency Services requirements. The governing body of the REH may also elect to grant nurse practitioners and physician assistants medical staff privileges in accordance with state scope-of-practice laws.
Is there a limit on the length of stay for patients at REHs?
Since Rural Emergency Hospitals are intended to provide outpatient care, they cannot exceed an annual average length of stay of 24 hours per patient. The length of stay begins at the time of registration, check-in, or triage of the patient, whichever occurs first, and ends upon discharge from the REH.
The Centers for Medicare & Medicaid Services (CMS) acknowledges that patients in need of inpatient psychiatric or rehabilitation services may need to remain at an REH for observation for several days or weeks if an inpatient bed is not immediately available. However, CMS noted in the July 2022 proposed rule that it does not anticipate that this circumstance will happen frequently enough to impact the annual average length of stay. In the November 2022 final rule, CMS stated that REHs are expected to maintain documentation on attempts to transfer patients and other reasons for extended lengths of patient stays. CMS will review and consider this information if the average annual patient length of stay exceeds 24 hours.
What kinds of agreements does an REH need to have with an acute care hospital?
An REH is required to have a transfer agreement with at least one Medicare-certified hospital designated as a level I or level II trauma center to ensure that patients can receive emergency medical care not available at the REH. The level I or level II trauma center does not have to be in the same state as the REH. REHs may also have agreements with hospitals that are not designated as level I or level II trauma centers.
Are Rural Emergency Hospitals eligible for the 340B program?
No. The 340B program allows certain eligible healthcare facilities to purchase prescription and non-prescription medications at reduced cost. The Consolidated Appropriations Act, 2021 (Public Law 116-260) that established the Rural Emergency Hospital program did not add REHs to the list of facilities eligible for the 340B program.
What are the quality assurance and quality improvement options for REHs?
Rural Emergency Hospitals must report data on selected Hospital Outpatient Quality Reporting Program measures for the REH Quality Reporting (REHQR) Program. Participation in the REHQR Program is used to assess compliance with program requirements. The REHQR program does not currently include an associated payment adjustment. Additional resources and support for REHQR are available through the Quality Reporting Center and the REH Technical Assistance Center.
What is the REH survey process?
An eligible facility converting to REH status that meets the Critical Access Hospital (CAH) or hospital Conditions of Participation (CoPs) that attests to meeting the REH CoPs will not receive an initial on-site survey. For facilities that were open and eligible to convert to an REH on December 27, 2020, but had since closed and re-enrolled in Medicare, they must receive an on-site survey by the state survey agency. The survey will verify that the facility meets the federal REH requirements. Details about the survey process are available in Appendix O of the CMS State Operations Manual, as presented in Revised: Guidance for Rural Emergency Hospital Provisions, Conversion Process and Conditions of Participation.
What sources of capital funding exist for REHs?
Rural Emergency Hospitals (REHs) may qualify for a variety of funding opportunities, such as grants and loans. For example, the following two federal programs focus on helping REHs with their capital funding needs:
- USDA Community Facilities Loan and Grant Program – Provides funding to construct, expand, or improve rural healthcare facilities, including REHs.
- HUD Section 242: Hospital Mortgage Insurance Program – Helps rural healthcare facilities finance new construction, refinance debt, or purchase new equipment such as hospital beds and office machines.
In addition to federal programs, state and local organizations may have their own funding initiatives for rural healthcare facilities.
Visit the funding section of this guide and the Capital Funding topic guide for additional federal, state, and foundation opportunities and information on capital funding in rural communities. REHs may also be eligible for funding found on our list of funding opportunities related to rural hospitals.
Who can I contact for technical assistance and support related to Rural Emergency Hospitals?
The Federal Office of Rural Health Policy funds the Rural Emergency Hospital Technical Assistance Center (REH-TAC) to support Critical Access Hospitals and other eligible rural hospitals that are considering conversion to Rural Emergency Hospital designation. The REH-TAC provides resources for broad dissemination to assist hospitals and communities in initial assessments of feasibility in converting. For hospitals and communities where the REH provider type is something to explore more in-depth, REH-TAC offers one-on-one technical assistance and support, such as financial analysis of REH conversion, assistance with the CMS application, and strategic planning guidance. Additionally, the FORHP Rural Hospital Technical Assistance Finder can help you identify free technical assistance opportunities that match your TA needs.
Other important contacts include:
- CMS Regional Office Rural Health Coordinator – for questions about CMS regulations
- State Survey Agency – for survey and certification questions
- Medicare Administrative Contractor (MAC) – for questions about Medicare claims, reimbursement, and billing issues
- State Rural Hospital Flexibility Program Contact – for state-level information about the REH provider type

