Healthcare Access in Rural Communities
Access to healthcare services is critical to good health, yet rural residents face a variety of access barriers. A 1993 National Academies report, Access to Healthcare in America, defined access as "the timely use of personal health services to achieve the best possible health outcomes." A 2014 RUPRI Health Panel report on rural healthcare access summarizes additional definitions of access with examples of measures that can be used to determine access.
Ideally, residents should be able to conveniently and confidently access services such as primary care, dental care, behavioral health, emergency care, and public health services. Access to healthcare is important for:
- Overall physical, social, and mental health status
- Disease prevention
- Detection, diagnosis, and treatment of illness
- Quality of life
- Avoiding preventable deaths
- Life expectancy
Rural residents often encounter barriers to healthcare that limit their ability to obtain the care they need. Access to healthcare implies that healthcare services are available and obtainable in a timely manner. Even when an adequate supply of healthcare services exists in the community, there are other factors that may impede healthcare access. For instance, to have healthcare access, rural residents must also have:
- Financial means to pay for services, such as health or dental insurance that is accepted by the provider
- Means to reach and use services, such as transportation to services that may be located at a distance, and the ability to take paid time off of work to utilize services
- Confidence in their ability to communicate with healthcare providers, particularly if the patient is not fluent in English or has limited health literacy
- Trust that they can use services without compromising privacy
- Confidence that they will receive quality care
This guide provides an overview of healthcare access in rural America, including the importance and benefits of healthcare access as well as the barriers that rural residents experience. The guide includes information regarding:
- Barriers to care, including workforce shortages, health insurance status, transportation issues, health literacy, and stigma in rural communities
- Access issues for specific populations and healthcare services
- Strategies and resources to improve access
Frequently Asked Questions
- How does the lack of healthcare access affect population health and patient well-being in a community?
- What are barriers to healthcare access in rural areas?
- Why is primary care access important for rural residents?
- What types of healthcare services are frequently difficult to access in rural areas?
- How do rural healthcare facility and service closures impact access to care?
- What are some strategies to improve access to care in rural communities?
- What can be done to help rural veterans access healthcare?
- What organizations work to improve rural healthcare access?
- How are private foundations working to improve healthcare access and the related reimbursement issues?
How does the lack of healthcare access affect population health and patient well-being in a community?
The supply of primary care providers per capita is lower in rural areas compared to urban areas, according to Supply and Distribution of the Primary Care Workforce in Rural America: 2019. Travel to reach a primary care provider may be costly and burdensome for patients living in remote rural areas, with subspecialty care often even farther away. These patients may substitute local primary care providers for subspecialists or they may decide to postpone or forego care. If patients do not have access to primary care or subspecialty care, they may use emergency department (ED) services for their healthcare needs. According to the 2024 article Non-Urgent Use of Emergency Departments by Rural and Urban Adults, 16% of rural adults compared to 13% of urban adults reported ED visits, and 5% of rural adults used the ED for a non-urgent reason compared to 4% of urban adults.
According to the 2014 RUPRI Health Panel report, Access to Rural Health Care - A Literature Review and New Synthesis, barriers to healthcare result in unmet healthcare needs, a lack of preventive and screening services, challenges in the treatment of chronic diseases, and even a reduced lifespan. While access to medical care does not guarantee good health, access to healthcare is critical for a population's well-being and optimal health.
The challenges that rural residents face in accessing healthcare services contribute to health disparities. To learn more about disparities in health outcomes, see the Rural Health Disparities topic guide.
What are barriers to healthcare access in rural areas?
Distance and Transportation
Rural populations are more likely to have to travel long distances to access healthcare services, particularly subspecialist services. This can be a significant burden in terms of travel time, cost, and time away from the workplace. In addition, the lack of reliable transportation is a barrier to care. In urban areas, public transit is generally an option for patients to get to medical appointments; however, these transportation services are often lacking in rural areas. Rural communities often have more elderly residents who have chronic conditions requiring multiple visits to outpatient healthcare facilities. This becomes challenging without available public or private transportation. The Transportation to Support Rural Healthcare topic guide provides resources and information about transportation and related issues for rural communities.
Workforce Shortages
Healthcare workforce shortages impact healthcare access in rural communities. One measure of healthcare access is having a regular source of care, which is dependent on having an adequate healthcare workforce. Other indicators, such as measures of nonuse that count rural residents who could not find an appropriate care provider, can further provide estimates of whether a sufficient healthcare workforce is available to rural residents. See What state-level policies and programs can help address the problem of shortages in the rural healthcare workforce? on the Rural Health Workforce topic guide for more information.
A shortage of healthcare professionals in rural areas of the U.S. can restrict access to healthcare by limiting the supply of available services. As of September 2024, 66.33% of Primary Care Health Professional Shortage Areas (HPSAs) were located in rural areas. For the most current numbers, see the Health Resource and Services Administration's (HRSA) Designated Health Professional Shortage Areas Statistics. HRSA also includes statistics on mental health and dental HPSAs.
Primary Care HPSAs are scored 0-25, with higher scores indicating a greater need for primary care providers. This January 2026 map highlights nonmetropolitan areas with primary care workforce shortages, with areas in darker green indicating higher nonmetro HPSA scores:
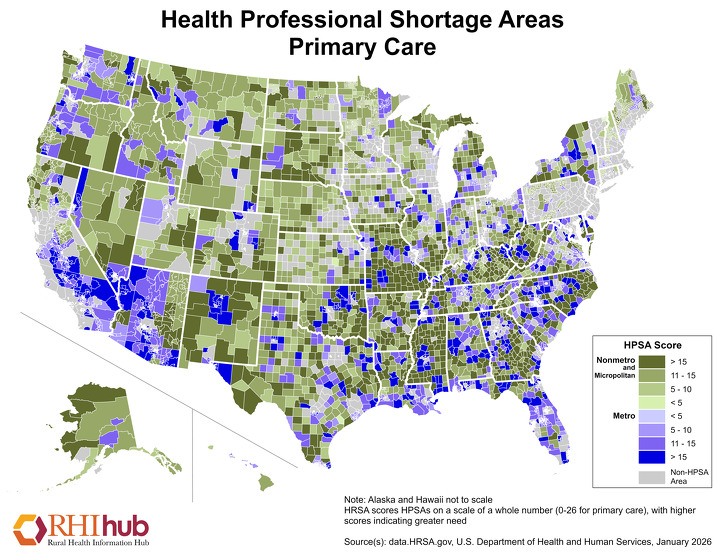
For more information on workforce challenges, resources, and strategies used to address rural healthcare workforce shortages, see the Rural Healthcare Workforce topic guide.
Health Insurance Coverage and Cost
Individuals without health insurance have less access to healthcare services. According to Geographic Variation in Health Insurance Coverage: United States, 2022, nonmetropolitan children and adults under 65 were more likely than their metropolitan peers to be uninsured.
| Urbanization Level | Adults, ages 18-64 | Children, ages 0-17 |
|---|---|---|
| Large central metropolitan | 13.9 | 3.9 |
| Large fringe metropolitan | 10.1 | 4.0 |
| Medium/small metropolitan | 12.2 | 4.0 |
| Nonmetropolitan | 13.9 | 5.5 |
| Source: Geographic Variation in Health Insurance Coverage: United States, 2022 | ||
The cost of healthcare can be an access barrier, and KFF reports that in 2022, 43% of adults postponed medical care for themselves or a household family member due to cost. This issue is often exacerbated in rural areas, with 12% of rural adults reporting they or a family member had difficulty paying medical bills, compared to 10% of urban adults. The 2023 policy brief, Rural Working-Age Adults Report More Cost Barriers to Health Care, states that rural working adults are more likely than their urban counterparts to report issues with paying medical bills or delaying care because of the cost. However, the cost of healthcare is an issue for both rural and urban residents.
Health insurance affordability is a concern for rural areas. A RUPRI Center for Rural Health Policy Analysis policy brief, Nonmetropolitan Premiums, Issuer Participation, and Enrollment in Health Insurance Marketplaces in 2022, evaluated unsubsidized and net-of-subsidy marketplace (HIM) plan premiums in 2022. Average premiums were higher in rural counties than in urban counties. In addition, rural counties were more likely to have fewer than 3 firms participating in the HIM. Medicare Advantage plan co-pays and deductibles are higher in rural, and no-cost benefits like health clubs and transportation are less frequently offered in rural areas. According to Changes in Marketplace Premiums and Insurer Participation, 2022-2023, rural areas tend to have fewer insurers and little competition among them, which can result in higher premiums.
Broadband Access
While the use of telehealth services was already becoming more popular and widespread at the beginning of 2020, measures implemented in response to the COVID-19 pandemic accelerated this growth. Unfortunately, many areas lack access to broadband internet and experience slow internet speeds, both of which are barriers to accessing telehealth services. According to Computer and Internet Use in the United States: 2021, 9.0% of urban households did not have a broadband subscription, compared to 13.4% of rural households. To learn about additional challenges for rural telehealth use, see What are the challenges related to providing telehealth services in rural communities? on the Telehealth and Health Information Technology in Rural Healthcare topic guide.
Health Literacy
Health literacy can also be a barrier to accessing healthcare. Health literacy impacts a patient's ability to understand health information and instructions from their healthcare providers. This can be especially concerning in rural communities, where lower educational levels and higher incidence of poverty often impact residents. Low health literacy can make residents reluctant to seek healthcare due to fear or frustration related to communicating with a healthcare professional. Additionally, navigating the healthcare system can be difficult without health literacy skills. To learn more about low health literacy in rural America, see the Rural Health Literacy Toolkit in our evidence-based toolkits. The Rural Monitor's 2017 two-part series on rural health literacy, Understanding Skills and Demands is Key to Improvement and Who's Delivering Health Information? explores connections between health and health literacy and how health information is being delivered to rural populations. The Rural Monitor's 2022 two-part series, A New Era of Health Literacy? Expanded Definitions, Digital Influences, and Rural Perspectives and Educating Future Healthcare Providers: Health Literacy Opportunities for Webside Manners explores health literacy in the digital era.
Social Stigma and Privacy Issues
In rural areas, because there is little anonymity, social stigma and privacy concerns are more likely to act as barriers to healthcare access. Rural residents can have concerns about seeking care for mental health, substance use, sexual health, pregnancy, or even common chronic illnesses due to unease or privacy concerns. Patient discomfort may be due to personal relationships with their healthcare provider or others working in the healthcare facility. Additionally, patients can feel fear or concerns about other residents, who are often friends, family members, or co-workers, who may notice them utilizing services for health conditions that are typically not openly discussed, such as counseling or HIV testing services. The 2024 article Identifying Challenges and Solutions for Improving Access to Mental Health Services for Rural Youth: Insights from Adult Community Members discusses stigma and barriers to mental healthcare in rural areas. Co-location or the integration of behavioral health services with primary care healthcare services in the same building can help ease patient concerns. Community programming that promotes positive mental health can destigmatize mental healthcare, and access to telemental health services may help alleviate privacy issues.
Why is primary care access important for rural residents?
Primary care, in addition to emergency care and public health services, is an essential rural healthcare service. Primary care providers offer a broad range of services and treat a wide spectrum of medical issues. The American Academy of Family Physicians characterizes primary care as follows:
“[…] primary care includes health promotion, disease prevention, health maintenance, counseling, patient education, diagnosis and treatment of acute and chronic illnesses in a variety of health care settings…A primary care practice serves as the patient's entry point into the health care system and as the continuing focal point for all needed health care services.”
A 2005 Milbank Quarterly article, Contribution of Primary Care to Health Systems and Health, identifies the key roles primary care access plays in preventing disease and improving health. Primary care serves as a first entry point into the health system, which can be particularly important for rural residents, who might otherwise face barriers to accessing healthcare. Some benefits of primary care access are:
- Preventive services, including early disease detection
- Care coordination
- Lower all-cause, cancer, and heart disease mortality rates
- Reduction in low birth weight
- Improved health behaviors
- Improved overall health
- Lower healthcare costs
Rural Healthy People 2030 discusses how residents with limited primary care access may not receive preventive screenings that can lead to early detection and treatment of disease, as well as missing opportunities for behavioral healthcare screening and initiation. Primary Care in the United States: A Chartbook of Facts and Statistics reports that preventive care visit utilization, which measures the number of residents who have preventive care visits in a given year, is 35% in rural areas, compared to 45% in urban areas.
What types of healthcare services are frequently difficult to access in rural areas?
Home Health
Home health services in rural America are a growing need but can be difficult to access for some rural residents. According to Exploring Access to Critical Health Services for Older Adults in Rural America from 1990 to 2020, access to home health agencies was highest in urban and higher population rural areas but declined in the most remote communities. Home is Where the Heart Is: Insights on the Coordination and Delivery of Home Health Services in Rural America, a 2017 Rural Health Reform Policy Research Center policy brief, covers many barriers and challenges facing rural home health agencies that affect their ability to provide access in rural areas, including:
- Reimbursement and insurance coverage
- Face-to-face requirement
- Homebound status requirement
- Changing rules and regulations
- Workforce
- Time and resources required to serve patients located at a distance
- Discharge process and referral difficulties
See To what extent are home health services available in rural communities? on the Rural Home Health Services topic guide for more information.
Hospice and Palliative Care
Hospice and palliative care agencies often face barriers and challenges similar to other healthcare services in rural areas. These challenges can include workforce shortages, recruitment and retention programs, reimbursement issues, limited access to broadband, and others.
The Rural Hospice and Palliative Care topic guide answers frequently asked questions and provides resources on hospice and palliative care in rural areas. Community-based Palliative Care: Scaling Access for Rural Populations, a 2018 Rural Monitor article, describes the role palliative care plays in meeting the needs of patients who are chronically and seriously ill and covers challenges to accessing palliative care in rural areas.
Mental Health Services
Access to mental health providers and services is a challenge in rural areas. As a result, primary care providers often fill the gap and provide mental health services. However, primary care providers may face challenges that limit their ability to provide mental health care access, such as inadequate financial reimbursement or lack of time with patients.
Rural communities face shortages in mental healthcare providers. As of September 2024, 61.85% of Mental Health Professional Shortage Areas were located in rural areas. For the most current figures, see HRSA's Designated Health Professional Shortage Areas Statistics.
Mental Health HPSAs are scored 0-25, with higher scores indicating a greater need for mental health providers. The January 2026 map below highlights mental health HPSAs for both metro areas, in multiple shades of purple, and nonmetro areas, in various shades of green.
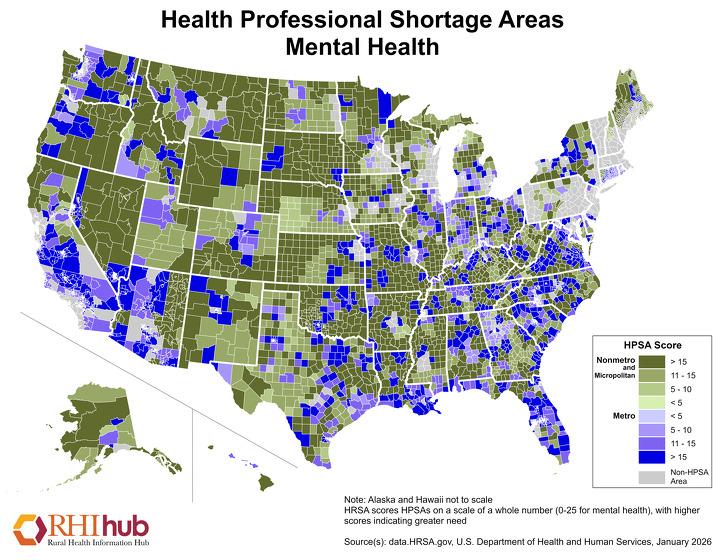
The 2023 report, Rural Health Research Recap: Rural Behavioral Health Workforce, summarizes research from Rural Health Research Centers that show how rural counties have fewer social workers, psychologists, psychiatric nurse practitioners, and counselors when compared to urban counties.
Due to the lack of mental health providers in rural communities, the use of telehealth to deliver mental health services is increasing. By using telehealth delivery systems, mental health services can be provided in a variety of rural settings, including rural clinics, schools, residential programs, long-term care facilities, and individual patient homes. Additionally, the Calendar Year (CY) 2022 Medicare Physician Fee Schedule Final Rule made permanent the ability for FQHCs and RHCs to be reimbursed by Medicare for telemental health appointments. The Telehealth and Health Information Technology in Rural Healthcare topic guide has many more resources on how telehealth can improve access to care. For additional resources on access to mental health services in rural areas, see the Rural Mental Health topic guide.
Substance Use Disorder Services
Despite a growing need, there is a shortage of substance use disorder services offered in many rural communities across America.
Medically managed withdrawal is an initial step of substance use disorder treatment that involves managing acute intoxication and withdrawal as well as minimizing medical complications. The lack of withdrawal management providers in many rural areas creates a barrier to care that could result in patients forgoing or delaying needed treatment. In lieu of a withdrawal management provider in a rural community, the local emergency room or county jail, although not the most appropriate location for withdrawal management services, must often serve as a substitute. The 2024 article Rural–Urban Differences in Out-of-Network Treatment Initiation and Engagement Rates for Substance Use Disorders reports similar issues, showing that there are lower rates of substance use treatment initiation and engagement in rural areas compared to urban areas.
Access to medication for opioid use disorder (MOUD) as well as medications for treating alcohol use disorder (MAUD) is also limited in rural communities. What's MAT Got to Do with It? Medication-Assisted Treatment for Opioid Use Disorder in Rural America provides an overview of using MOUD as part of evidence-based treatment for opioid use disorder, with information on the science behind the disorder and how 3 medications for opioid use disorder (Buprenorphine, Methadone, and Naltrexone) work. According to Practical Tools for Prescribing and Promoting Buprenorphine in Primary Care Settings, rural areas benefit from using the drug buprenorphine for MOUD treatment, but often face staffing, transportation, and technology constraints that prevent making MOUD a viable option in rural communities. This publication provides recommendations to improve access, such as leveraging non-physician staff for treatment and engaging the local community to build service locations as strategies to overcome barriers. In addition, the publication suggests: "Prescribe buprenorphine products that patients can use at home or over extended periods of time to support patients who face barriers related to traveling. Home induction is a feasible and safe method of initiating buprenorphine treatment for many patients."
A shortage of mental health and substance use disorder clinicians in rural communities led to the development of new models to bridge the gap and provide needed mental health and substance use disorder services using allied behavioral health workers. Some examples include:
- Nurse Navigator and Recovery Specialist Outreach Program
- ASPIN Network's Community Health Worker Program
The Substance Use and Misuse in Rural Areas and Rural Response to the Opioid Crisis topic guides provide information and resources, answer frequently asked questions, and list model programs to address substance use disorder and model programs to address opioid use in rural areas.
Reproductive, Obstetric, and Maternal Health Services
Reproductive healthcare is typically more difficult to access in rural areas. According to the Kaiser Family Foundation's (KFF) issue brief, Women's Sexual and Reproductive Health Services: Key Findings from the 2020 KFF Women's Health Survey, rural women are less likely to have had a recent pap test and less likely to have access to a provider who discussed reproductive health issues with them, such as contraception, sexual and relationship history, sexually transmitted infections (STIs) and other transmissible diseases, pre-exposure prophylaxis (PrEP), and menopause.
Access to obstetric services is a persistent, but growing concern in rural areas. A 2022 Center for Economic Analysis of Rural Health policy brief, County-Level Availability of Obstetric Care and Economic Implications of Hospital Closures on Obstetric Care, reports that out of 148 counties that lost obstetric services between 2012 and 2019 due to hospital or unit closures/conversions, 113 of the counties were rural. Additionally, a 2020 action plan from the U.S. Department of Health and Human Services, Healthy Women, Healthy Pregnancies, Healthy Futures: Action Plan to Improve Maternal Health in America, points out that, although 15% of people in the U.S. live in rural communities, only 6% of OB/GYNs serve these areas. However, many rural family physicians provide broad OB/GYN services to their patients.
A 2020 case study Making it Work: Models of Success in Rural Maternity Care discusses 3 rural obstetric service providers, highlighting the importance of strong partnerships, collaboration, and community support to maintaining successful rural maternity care. The Rural Maternal Health Toolkit also discusses access to maternity care in rural areas.
The 2019 National Rural Health Association (NRHA) policy brief, Access to Rural Maternity Care, provides an overview of the decline in access to maternity care in rural areas and factors contributing to the decline in access. The brief offers policy considerations to support maternity care services and address barriers to access in the rural U.S., such as increasing research funding, rural OB practice challenges, workforce issues, and quality of OB care. The report Restoring Access to Maternity Care in Rural America discusses strategies to improve maternal care, such as creating maternity care networks, promoting visibility for care, helping rural providers care for patients with high-risk pregnancies, utilizing telemedicine, expanding and training the rural healthcare workforce, enlisting nonclinical partners, and more. For more information on rural maternal health issues and strategies to address them, see the Rural Maternal Health topic guide.
Oral Health Services
Oral health can affect overall physical and emotional health. For example, oral health needs that are not addressed can lead to pain or cosmetic concerns that can affect academic or professional success. Despite the importance of oral health, access to dental care is either very limited or difficult to access in many rural and remote communities.
Traditionally, health insurance plans have not covered oral health services. A separate dental insurance plan is needed to cover oral health services and procedures. According to the 2021 National Institutes of Health report Oral Health in America, fewer rural residents have dental insurance compared to urban residents.
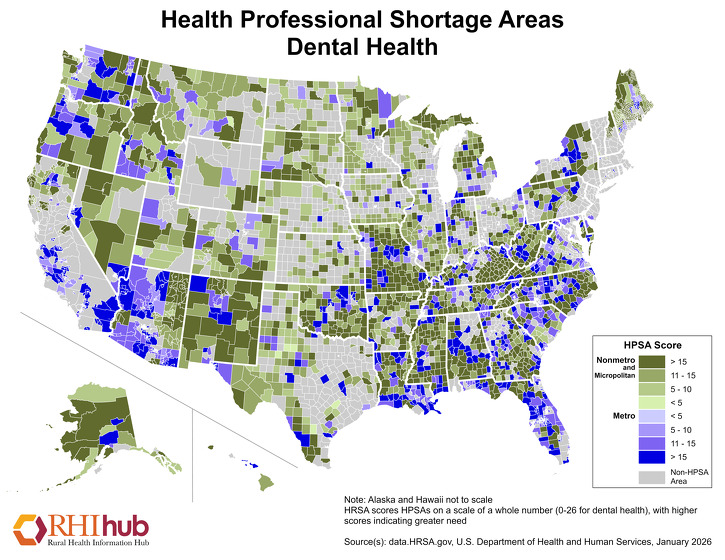
Another factor limiting access to dental services is the lack of dental health professionals in rural and underserved areas. As of September 2024, 66.70% of Dental Health Professional Shortage Areas were located in rural areas. For the most current numbers, see HRSA's Designated Health Professional Shortage Areas Statistics. According to 2020-2021 HRSA Area Health Resource Files, there are 7.5 dentists per 10,000 citizens in metropolitan areas and 4.7 dentists per 10,000 citizens in nonmetropolitan areas. The lack of dental professionals in rural areas can lead to poor oral health in rural residents.
Dental Health HPSAs are scored 0-26, with higher scores indicating a greater need for dental health providers. This January 2026 map highlights nonmetropolitan areas with dental health workforce shortages, with areas in darker green indicating higher nonmetro HPSA scores:
A May 2018 NRHA policy brief, Improving Rural Oral Healthcare Access, offers recommendations to address dental workforce shortages and to ultimately improve access to oral health services, including:
- Providing rural training tracks during dental education
- Admitting dental students from rural areas who would be more likely to practice in a rural community
- Providing dental students opportunities to obtain a broad range of dental skills which will be needed in a rural practice
- Helping rural communities recruit and retain oral health providers through local community development programs
For more information, see What oral health disparities are present in rural America? on the Oral Health in Rural Communities topic guide.
How do rural healthcare facility and service closures impact access to care?
The closure of rural healthcare facilities or the discontinuation of services can have a negative impact on access to healthcare in rural communities. Local rural healthcare systems are often fragile; when one facility closes or a provider leaves, it can impact care and access across the community. For example, if a surgeon leaves, C-section access declines and obstetric care is jeopardized. If a hospital closes, it may be harder to recruit physicians.
There are multiple factors that can affect the severity and impact of a hospital or healthcare facility closure on healthcare access, including:
- Distance to the next closest provider
- Availability of alternative services
- Transportation services
- Community members' socioeconomic and health status
Traveling to receive healthcare services places the burden on patients. For individuals with low incomes, no paid time off from their jobs, physical limitations, acute conditions, or no personal transportation, these burdens can significantly affect their ability to access healthcare services.
Hospital closures create access issues for rural residents. A 2015 findings brief from the North Carolina Rural Health Research Program, A Comparison of Closed Rural Hospitals and Perceived Impact, identifies the following potential impacts on healthcare access due to hospital closure:
- Unstable health services, particularly diagnostic and lab tests, obstetrics, rehabilitation, and emergency medical care
- Rising EMS costs
- Residents not receiving needed care or services due to lack of transportation
- Greater impact on access for the elderly, the poor, people with disabilities, and other groups in need
The North Carolina Rural Health Research Program maintains an interactive map that displays locations of rural hospital closures in the U.S. from January 2005 to present. According to the map, 106 rural hospitals have completely closed since 2005, and 86 have converted to a different form of healthcare facility. Unfortunately, rural health experts believe rural hospital closures are likely to continue because many rural hospitals have minimal operating margins with little room for financial loss.
A significant concern for rural communities losing their hospital is the loss of emergency services. In emergency situations, care delays can have serious adverse consequences on patient outcomes. Alternative models and provider types may be needed to meet access needs in rural areas in the event of closures. A 2016 Medicare Payment Advisory Commission presentation, Improving Efficiency and Preserving Access to Emergency Care in Rural Areas, describes policies and strategies to ensure access to emergency department services in rural areas. The presentation provides discussion on alternative healthcare delivery models. The 2020 research brief, Alternatives to Hospital Closure: Findings from a National Survey of CAH Executives, explores options to maintain access in rural communities whose hospitals are encountering negative profit margins. Starting in 2023, converting to a Rural Emergency Hospital (REH) is an option for rural hospitals as an effort to maintain some emergency services in rural areas. For more information, see the Rural Emergency Hospitals topic guide.
Additional closures impacting rural areas can be seen in nursing homes in nonmetropolitan counties. Trends in Nursing Home Closures in Nonmetropolitan and Metropolitan Counties in the United States, 2008-2018 shows that in this time span 472 nursing homes closed in 400 nonmetropolitan counties and as of 2018, 10.1% of rural counties in the U.S. were considered nursing home deserts. According to Nursing Home Closures and Trends: June 2015 - June 2019, the impact of closure is significant for rural communities, who have fewer options for nursing home care and rely on healthcare facilities as centers for employment. Nursing Home Closures and Access to Post-Acute Care and Long-Term Care Services in Rural Areas states that rural areas experiencing closures have longer distances to travel to the next available nursing home offering post-acute care, an average of 6.4 miles compared to 0.94 miles for urban areas. The article shows similar results for long-term care services, with 7.2 miles of travel for rural areas and 1.1 miles for urban areas.
Maintaining pharmacy services in rural towns can also be a challenge, particularly when the only pharmacist in town nears retirement. When a community's only pharmacy closes, it creates a void and residents must adapt to find new ways to meet their medication needs. Closures can be difficult for older patients or people with disabilities who rely on pharmacy care to assist in managing their medications.
A 2024 data brief from RUPRI Center for Rural Health Policy Analysis, Changes in Rural Pharmacy Presence 2023, describes rural communities that lost pharmacy services between 2018 and 2023:
- 20.5% of the population was aged 65 and older
- Unemployment was at 3.9%
- Uninsured rates were 9.2%
- 17.8% were impoverished
- 17.6% were living with a disability
The 2024 article, Locations and Characteristics of Pharmacy Deserts in the United States: A Geospatial Study, states that locations considered pharmacy deserts are more likely to have a population with lower educational attainment, have lower rates of insurance coverage, fewer English-speaking residents, more residents with an ambulatory disability.
A 2022 RUPRI Center for Rural Health Policy Analysis Brief states: "Between 2003 and 2021, the number of retail pharmacies declined in noncore rural areas by 9.8 percent, and in rural micropolitan areas by 4.4 percent, while the number in metropolitan areas increased by 15.1 percent during the same period." For more information on rural pharmacy access or challenges rural pharmacies face, see the Rural Pharmacy and Prescription Drugs topic guide.
What are some strategies to improve access to care in rural communities?
There are multiple strategies being used to improve access to healthcare in rural areas. Examples include:
Delivery Models
In 2023, a new Medicare provider type was implemented, the Rural Emergency Hospital, which is designed to maintain access to emergency and outpatient care in rural areas. For more information, see the Rural Emergency Hospital topic guide.
Community Paramedicine is a model of care in which paramedics and emergency medical technicians (EMTs) operate in expanded roles to assist with healthcare services for those in need without duplicating available services existing within the community. The Community Paramedicine topic guide describes how this model of care can benefit rural communities and covers steps to starting a rural community paramedicine program. Rural communities looking to develop community paramedicine or mobile integrated health programs can also view the Rural Community Paramedicine Toolkit for emerging practices and resources.
The Community Health Worker (CHW) model facilitates healthcare access by using CHWs as a liaison between healthcare providers and rural residents to ensure their healthcare needs are met. The Community Health Workers in Rural Settings topic guide offers information and resources on CHWs and covers CHW education, training, and certification.
Care coordination and team-based care models, such as Accountable Care Organizations (ACOs) and Patient-Centered Medical Homes (PCMHs), can also extend access to primary care services in rural communities. A variety of rural medical home and care coordination programs are highlighted in the Rural Health Models and Innovations section.
Affiliation with Larger Systems or Networks
Local rural healthcare facilities may choose to join healthcare networks or affiliate themselves with larger healthcare systems as a strategic move to maintain or improve healthcare access in their communities. These affiliations or joining of healthcare networks may improve the financial viability of the rural facility, provide additional resources and infrastructure for the facility, and allow the rural healthcare facility to offer new or expanded healthcare services they could not otherwise provide. However, the benefits of an affiliation with a larger healthcare system may come at the expense of local control.
The 2018 RUPRI Center for Rural Health Policy Analysis report, The Rural Hospital and Health System Affiliation Landscape – A Brief Review, discusses the various types of hospital affiliations that rural hospitals might consider and factors that might affect which option rural hospitals choose, such as maintaining local decision-making authority and meeting the demands of the hospital system affiliation. The report covers some benefits hospital system affiliation can afford a rural hospital, including access to:
- Technology
- Staff recruitment and retention
- Group purchasing
- Increased access to healthcare and operational services
- Ability to adapt to value-based payment models
- Improved performance
For facilities and providers who wish to remain independent, networks are a way to collaborate to create economies of scale and work toward mutual goals. Networks allow for the sharing of resources, group purchasing, and shared services, among other activities. Clinically integrated networks (CINs) are complex organizations that extend their collaborations into the clinical realm, creating efficiencies and quality care by working together and holding each other accountable to achieve mutual goals. For more information on these strategies, see the Rural Monitor article, Better Together: Rural Hospital High-Value Networks.
Efforts to Improve the Workforce
An adequate workforce is necessary for maintaining healthcare access in a community. In order to increase access to healthcare, rural communities must use their healthcare professionals in the most efficient and strategic ways. This might include allowing each professional to work at the top of their license, using new types of providers, working in interprofessional teams, and creative scheduling to offer clinic time outside of regular work hours. The 2024 report Access to Health Care in Rural America: Current Trends and Key Challenges features a variety of federal workforce programs that address healthcare workforce issues in rural communities. The Rural Healthcare Workforce topic guide discusses how rural areas can address workforce shortages, such as partnering with other healthcare facilities; increasing pay for staff; adding flexibility and incentives to improve recruitment and retention of healthcare providers; and using telehealth services. The guide also discusses state and federal policies and programs to improve the supply of rural health professionals, such as loan repayment programs and visa waivers.
Telehealth
Telehealth is considered to be a key tool to help address rural healthcare access issues. Through telehealth, rural patients can see subspecialists in a timely manner while staying in the comfort of their home or local facility. Local healthcare providers can also benefit from subspecialists' expertise provided via telehealth. However, there is the potential for unequal access to these services due to a lack of broadband internet access in some rural areas. The 2022 article Geospatial Analysis of Access to Health Care and Internet Services in the US shows that though counties with internet access were positively correlated with more available healthcare access, rural counties had less internet availability and were more likely to be situated in a healthcare desert. According to the Federal Communications Commission 2020 Broadband Deployment Report, 22.3% of rural Americans and 27.7% of Americans living in tribal areas lack fixed terrestrial broadband coverage, compared to 1.5% of Americans who lack coverage in urban areas.
An additional concern is the potential that access to telehealth services may supplant, rather than support, primary and subspecialist care in hard-to-reach areas, causing unintended consequences to healthcare facilities in rural areas. Financial Effects of Remote Product Delivery: Evidence from Hospitals draws attention to this concern, discussing issues such as loss of patient volume and financial burdens in rural hospitals due to distant providers acquiring rural patients through telehealth. Improving healthcare access in rural areas requires a balance of telehealth options and sustainable in-person healthcare.
For more information on telehealth policy, including broadband infrastructure, see the Rural Policy Research Institute's 2023 report, The Role of Telehealth in Achieving a High Performing Rural Health System: Priorities in a Post-Pandemic System. Additionally, the U.S. Department of Health and Human Services has a telehealth guide that is specific to rural areas as well as a telehealth policy page that provides the most recent information on telehealth policy.
The Telehealth and Health Information Technology in Rural Healthcare topic guide provides a broad overview of how telehealth is being used in rural communities to improve healthcare access. The guide covers specific programs currently in use in rural areas, as well as providing resources and a listing of funding and opportunities that can be used to support telehealth solutions.
What can be done to help rural veterans access healthcare?
One of the primary barriers that rural veterans face when accessing healthcare services is the significant travel distance to the nearest Veterans Affairs (VA) healthcare facility. A 2018 study found that rural veterans' access to healthcare is not necessarily an issue of eligibility for purchased care from non-VA providers, as most VA healthcare facility deserts also have shortages of non-VA providers. The 2024 U.S. Senate Committee on Veterans' Affairs hearing, Frontier Health Care: Ensuring Veterans' Access No Matter Where They Live, discusses issues related to rural veteran healthcare access, such as staffing, broadband, distance to healthcare providers, and more.
According to the 2019 research brief Access to Care Among Rural Veterans, 56% of rural veterans enrolled in the VA health system are over 65 years of age and are more likely to experience diabetes, heart conditions, and high blood pressure compared to urban veterans. Moreover, suicide rates are higher for rural compared to urban veterans. It is important that populations with complex medical needs have access to support programs.
To address access issues for rural veterans, the VA has created community-based outpatient clinics in many rural areas, in addition to using mobile clinics and telehealth services. To learn more about VA services for rural veterans or the VA's efforts to address veterans' healthcare access, see the Rural Veterans and Access to Healthcare topic guide.
What organizations work to improve rural healthcare access?
Many organizations work to meet the needs of rural communities and help ensure the availability of essential healthcare services.
- The Federal Office of Rural Health Policy (FORHP) focuses on rural healthcare issues and is part of HRSA.
- Rural Health Research Centers are funded by the Federal Office of Rural Health Policy to produce policy-relevant research and analysis on healthcare and issues impacting healthcare in rural areas.
- The Centers for Disease Control and Prevention (CDC) Office of Rural Health focuses on integrating rural health approaches and science into CDC programs while advancing rural public health strategies.
- The National Rural Health Association (NRHA) provides leadership and resources on rural health issues for healthcare providers and organizations working to improve the health of rural communities.
- The National Association of Rural Health Clinics (NARHC) works to improve the delivery of quality, cost-effective healthcare in rural areas through the RHC Program.
- The American Hospital Association (AHA) Section for Rural Health Services represents the interests of small and rural hospitals and works to ensure that the unique needs of this segment of AHA's membership are a national priority.
- State Offices of Rural Health (SORHs) and State Rural Health Associations (SRHAs) help rural communities build healthcare delivery systems by coordinating rural healthcare activities in the state, collecting and disseminating information, and providing technical assistance to public and nonprofit entities.
- The National Organization of State Offices of Rural Health (NOSORH) works to foster and promote legislation, resources, and education with the SORHs, FORHP, NRHA, and other organizations promoting and supporting rural healthcare access.
- The National Rural Recruitment and Retention Network (3RNET) is a national recruitment organization for healthcare professional jobs in rural communities.
How are private foundations working to improve healthcare access and the related reimbursement issues?
Many private foundations work to improve healthcare access by funding transportation services, improving workforce, and addressing other factors that affect rural healthcare access. Investing in existing safety net providers and programs, offering grants to develop and implement innovative healthcare delivery models, and funding research to study policy implications as they relate to rural healthcare access are all examples of actions foundations can take to support rural healthcare access.
A 2017 article published in Health Affairs, Foundations' Efforts to Improve Rural Health Care, covers private foundation projects focused on improving access to rural healthcare.
Grantmakers in Health offers multiple resources that provide education and guidance to foundations interested in improving rural healthcare access, such as Improving Health Care Access: Grantmakers Share Their Experiences and Improving Health Access in Communities, Lessons for Effective Grantmaking.