Vermont Hub-and-Spoke Model of Care for Opioid Use Disorder
- Need: In the early 2010s, needed increase access to medication treatment for opioid use disorder in rural Vermont.
- Intervention: 2012-2016 implementation of a statewide hub-and-spoke treatment access system.
- Results: The original system's increased treatment capacity and care coordination successes now are a permanent system of integrated care overseen by the Vermont state health department and Vermont Blueprint for Health.
Evidence-level
Effective (About evidence-level criteria)Description
With over 9,000 square miles, Vermont has a significant rural population. Of the state's 15 hospitals, eight are designated as Critical Access Hospitals. Although in the mid-2010s, Vermont was a national leader for its number of waivered providers for office-based opioid treatment (OBOT) of opioid use disorder (OUD), the state's providers were treating limited numbers of patients due to treatment-related challenges and lack of behavioral health partners. At the time, additional treatment barriers to medication-assisted treatment (MAT) for OUD — now known as medication for opioid use disorder (MOUD) — were provider reimbursement concerns as well as drug diversion challenges.
To address these issues for rural areas as well as for the entire state, the Care Alliance for Opioid Addictions Initiative (2012-2016) was created by the state's addiction medicine specialists and public health leaders. Original funding for that treatment model leveraged reimbursement through aspects of the Affordable Care Act's Home Health Services' Community Health Teams. Additional grant support came from the National Institutes of Health and the National Institute of General Medicine Science.
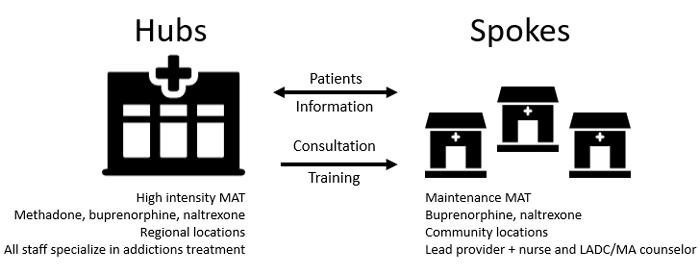
The Initiative designed an original model that implemented "spoke" OBOT connected to "hub"-based opioid treatment programs (OTP). Key to the project model was leveraging chronic disease management models that, at the time, were similar to other medical conditions. For example, congestive heart failure clinics staffed by cardiologists or HIV clinics with infectious disease specialists. Modeling this approach, addiction medicine specialists were located in hub specialty clinics that could match client needs of specialty-level expertise. Care coordination within those hub clinics linked a hub-spoke care coordination model for easier access to hub care when spoke teams identified the need for a higher level of care.
By 2017, Vermont had the highest capacity in the U.S. for treating OUD. A decade later, now this hub and spoke model continues with nine regional hubs and at 75 spoke locations, several hundred providers are providing MOUD care that is fully integrated into general healthcare.
Currently, hubs are overseen by Vermont's state department of health and spoke oversight occurs through Vermont's Blueprint for Health, Vermont's unique state-level plan that includes community-led strategies for improving health and well-being. In 2025, specific details of the current program can found in the state's online Blueprint for Health Manual, 2025.
Services offered
Detailed description of the current program's organization and treatment expectations are available through online access of the Vermont Blueprint for Health Manual, 2025. In brief summary, some of the program elements are:
Hubs:
- Located in 9 areas throughout state
- Employs addiction specialists to provide
specialty-level expertise at any time during the recovery
process as needed for some people
- These providers also provide training and consultation for spoke providers
- Provide Health Home services that include case management, care coordination, transition of care management, family support services, health promotion, and referral to community services.
Spokes:
- Primary care providers, obstetrics and gynecology providers, and chronic pain practices offer treatment and referral as an integrated service within general medical care. Spoke specialty outpatient addictions programs also available.
Results
According to a 2022 state report, more than 6,000 people were participating in recovery services. Academic articles offer further information on qualitative and quantitative program results.
Data from early implementation:
During the 2012-2016 implementation phase: Pre-implementation MAT wait times varied within the state. Within the 3-year implementation phase, very few people awaited treatment.
At the time when MAT participation required provider medication waiver requirements, qualified providers increased from numbering 173 to 283, and 50% increase in providers caring for more than 10 patients.
Other successes of early implementation that led to the program's ongoing success and sustainability were:
- Three years after program implementation, total Vermonters receiving MOUD number nearly 8,600 and no clients waited for hub services.
- Between the first quarter of 2016 and first quarter 2020, the state experienced nearly a 50% decrease of opioid prescriptions as measured in MME — morphine milligram equivalents — the method experts use to standardize opioid prescription use.
- With regards to the efforts addressing the incarcerated population's needs: With Act 176 passed in 2018, by Feb 2019, 16% of all inmates were receiving OUD care and by following November, nearly 50% of about 1500 previously incarcerated individuals were still receiving treatment.
For more program details see:
Online access of the Vermont Blueprint for Health Manual, 2025.Academic publications:
Hichborn, E. G., Murray, O. B., Murphy, E. I., Gallant, T. E., Moore, S. K., McLeman, B. M., Saroyan, J., Folland, A., Mitchell, M., & Marsch, L. A. (2025). Patient centered medication treatment for opioid use disorder in rural Vermont: a qualitative study. Addiction Science & Clinical Practice, 20(1), 3.
Nowak, S. A., Harder, V. S., Villanti, A. C., Heil, S. H., & Sigmon, S. C. (2023). Statewide Trends in Buprenorphine Prescribing in Rural and Nonrural Vermont: Analysis of Population-based Patient Pharmacy Claims. Journal of Addiction Medicine, 17 (6), 714–716.
Rawson, R., Cousins, S., McCann, M., Pearce, R., Van Donsel, A.. (2019) Assessment of medication for opioid use disorder as delivered within the Vermont hub and spoke system. Journal of Substance Abuse Treatment; 97:84-90. [Abstract.]
Brooklyn, J.R., Sigmon, S.C. (2017). Vermont Hub-and-Spoke Model of Care For Opioid Use Disorder: Development, Implementation, and Impact. Journal of Addiction Medicine; 11(4):286–292.
Vermont Hub-and-Spoke Model of Care for Opioid Use Disorders: An Evaluation. Richard A. Rawson. Vermont Center on Behavior & Health, The University of Vermont. December 2017.
Collaborative Models for Medication-assisted Treatment Key Elements of Vermont's Hub-and-Spoke System. Medicaid Innovation Accelerator Program, April 2019.
Vermont Results First Inventory and Benefit-Cost Analysis. Crime Research Group, December 2017.
Challenges
Initial implementation challenges were staffing shortages and data collection efforts across treatment network. With current oversight, data collection is part of required program reporting, including HEDIS (Healthcare Effectiveness Data and Information Set) measures.
Replication
Some of the original 2012-2016 Alliance replication recommendations still have continued value for any similar efforts today if considering a similar program in other states or regions:
- Involve passionate physician leaders
- Understand that spoke MOUD teams are integral to achieving success
- Provide education for policy makers
- Consider use of initial Learning Collaboratives to promote common language central to achieving project goals
- Partner with lead sections within a state's health department that's committed to providing comprehensive MOUD access
Contact Information
John R. Brooklyn M.D., Clinical Assistant ProfessorDepartment of Psychiatry, The University of Vermont
johnr.brooklyn@gmail.com
Topics
Access
· Illicit drug use
· Prescription drug misuse
· Service delivery models
· Substance use and misuse
States served
Vermont
Date added
June 13, 2018
Suggested citation: Rural Health Information Hub, 2025 . Vermont Hub-and-Spoke Model of Care for Opioid Use Disorder [online]. Rural Health Information Hub. Available at: https://www.ruralhealthinfo.org/project-examples/1015 [Accessed 6 March 2026]
Please contact the models and innovations contact directly for the most complete and current information about this program. Summaries of models and innovations are provided by RHIhub for your convenience. The programs described are not endorsed by RHIhub or by the Federal Office of Rural Health Policy. Each rural community should consider whether a particular project or approach is a good match for their community’s needs and capacity. While it is sometimes possible to adapt program components to match your resources, keep in mind that changes to the program design may impact results.
