Jun 30, 2021
Pulmonary Rehabilitation: Benefiting Rural Individuals, Benefiting Rural Population Health
Clinical lung specialists across the globe have seen the benefits up close for years. Patients with chronic obstructive pulmonary disease (COPD) and other chronic lower respiratory diseases have experienced the benefits personally. If referred and if a program is available, the benefits gained from pulmonary rehabilitation (PR) are as important for rural patients with chronic lung disease as cardiovascular rehabilitation programs are for patients with heart and blood vessel problems. In recent years, clinicians and researchers have come to recognize PR's benefits — especially for patients with COPD that have been recently hospitalized for "exacerbations" compared with the traditional philosophy that PR was most beneficial for medically stable patients.
New research results in 2020 further endorse the benefits: a diminished mortality rate. Analyzing 2014-2015 Medicare claims data of beneficiaries older than 65, researchers found that "Among fee-for-service Medicare beneficiaries hospitalized for COPD, initiation of pulmonary rehabilitation within 3 months of discharge was significantly associated with lower risk of mortality at 1 year."
How much lower? Nearly 40%.
Defining COPD Exacerbations and Pulmonary Rehabilitation

Source: National Heart, Lung, and Blood Institute
Researchers and clinicians define a COPD exacerbation as "an event in the natural course of the disease characterized by a change in the patient's baseline dyspnea, cough, and/or sputum and beyond normal day-to-day variations, that is acute in onset and may warrant a change in regular medication in a patient with underlying COPD." Exacerbations frequently require hospitalization, and post-discharge patients have been described as "experiencing a self-reinforcing spiral of dyspnea-related deconditioning."
The American Thoracic Society and European Respiratory Society define PR as "a comprehensive intervention based on a thorough patient assessment followed by patient tailored therapies that include, but are not limited to, exercise training, education, and behavior change, designed to improve the physical and psychological condition of people with chronic respiratory disease and to promote the long-term adherence to health-enhancing behaviors." Based on the severity of COPD as determined by spirometry, federal regulations specify Medicare conditions for coverage of PR services.
PR: Unfortunately, A Well-Kept Secret
For over 30 years, registered nurse Gayla Oakley has seen members of her community with chronic lower respiratory diseases benefit from the tailored PR program offered through the local Critical Access Hospital in Albion, Nebraska. She expressed concern that far too few rural patients can access PR. According to research published in 2019, less than 30% of noncore counties have PR, in contrast to over 50% of metro- and micropolitan counties. Additionally, the report pointed out that only around 35% of Critical Access Hospitals have programs.

"Unfortunately, pulmonary rehab's like the best-kept secret," Oakley said. "It's so effective, yet under-prescribed. And it's not just the patients themselves whose lives are dramatically changed, but their families' lives are changed too when they see their loved one with COPD or another lung condition feel so much better and regain some independence. Patients will say, 'I've had this lung disease for five, ten, 15 years. Why hasn't anyone told me about pulmonary rehab? Or 'I was told that I couldn't exercise because I was on oxygen and that I needed to conserve my energy.' After they're in the program, patients and their families are just so amazed about how program elements like breathing retraining and understanding how to take medications correctly can make such a difference."
More in This Series
In part 1 of this 2-part series on rural COPD issues, read about the impact of the COPD National Action Plan in the Rural Monitor's Still Stealing Rural America's Breath: An Update on Chronic Obstructive Pulmonary Disease.
Oakley, the director of the cardiac and pulmonary rehabilitation programs in Albion, said she is passionate about advocating for PR offerings in rural areas. In her current local directorship role and her leadership role with the American Association of Cardiovascular and Pulmonary Rehabilitation (AACVPR), she will connect with peers in small and rural organizations interested in starting new programs. Because every rural area has a unique need, she recommends those considering a new PR program should check with an AACVPR state or regional affiliate who will likely be able to provide insight on start-up issues.
Tele-Pulmonary Rehabilitation: Potential for Increasing Rural PR Access?
The forced move to the increased use of telehealth during the COVID-19 pandemic has provided care to many people — especially in rural areas — who otherwise would have received little or even no care at all. However, the effectiveness and value of telehealth during this public health emergency (PHE) came as no surprise to many experts who've long understood its value for the evaluation and treatment of many physical and mental health conditions. Though some experts note that telehealth can't increase capacity, it can at least increase access to care. For the hundreds of thousands of rural patients with COPD and other chronic lower respiratory diseases, providing access to PR through either a virtual home-based program or a virtual program in a rural inpatient or outpatient setting could offer the benefits of increased quality of life — and in view of recent research — perhaps even a longer life.
Prior to the PHE, researchers were already involved with studying the effectiveness of remotely-delivered PR. Noting the limited availability of rural PR programs, University of California San Francisco specialists discussed infrastructure needs and required strategies for moving pulmonary rehabilitation into patient homes and stated in their 2018 clinical review, "The future of technology-supported, home-based PR in many ways appears limitless, given the remarkable advances and speed of development of medical technology." In 2019, researchers at the University of Alabama in Birmingham noted their home video telehealth PR program was one of the first to demonstrate decreased readmission rates within their healthcare system, an important initial finding considering that hospitalizations for COPD exacerbations account for two-thirds of the healthcare costs associated with the disease.
Including those patients with COPD — both diagnosed and undiagnosed — researchers have estimated that approximately 50% of patients with severe COVID-19 will require rehabilitation following hospital discharge. In 2021, experts in the United Kingdom specifically addressed COVID-related pulmonary rehabilitation needs stating that "online-PR improves patient outcomes and is feasible and acceptable for individuals referred for face-to-face PR in the context of a requirement for social distancing."
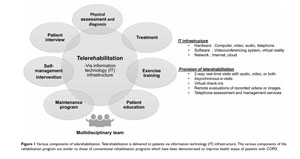
Experts also pointed out that, to date, research shows that tele-rehabilitation program components are similar to those of conventional rehabilitation programs. These components include a multidisciplinary team to provide assessment and treatment in addition to education around disease self-management. In their 2021 paper suggesting tele-PR be the new standard for COPD patients, Canadian researchers stated that now, more than ever, these programs need "solid high-quality evidentiary data" for policymaking decisions.

Given the need to increase access to PR programs, Dr. Antonello Punturieri, program director in the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, part of the National Institutes of Health, said that more tele-PR research activities are underway in the U.S. with rural populations in mind.
"The COVID-19 pandemic has forced the engineering of new ways of delivering care, including care delivered in hard-to-reach areas," he said. "PR is now a focus of several research projects experimenting with tele-PR implementation. We know that PR could make a difference for patients with COPD in rural America."
New Rural PR Programs: Eye on Population Health
Despite limitations due to reimbursement and delays as a result of the COVID-19 public health emergency, healthcare organizations in Nebraska and Michigan have added new PR programs, citing their efforts as beneficial to population health management in addition to benefits for individual patients.

Arlan Johnson, CEO of Howard County Medical Center (HCMC) in St. Paul, Nebraska, said that the decision to start PR at their facility was based on personal awareness of occupational lung diseases in rural areas, hearing the voice of a strong PR advocate at a national rural health meeting, and helpful rural-specific how-to information, for example the National Rural Health Resource Center's A Rural Hospital Guide to Improving Chronic Obstructive Pulmonary Disease. As a member of a rural Accountable Care Organization (ACO), he said he was also aware of PR's impact on resource utilization and, more importantly, the evidence that it has impact on patients' well-being and functional status.
Mandatory Components of a Pulmonary Rehabilitation Program
- Physician-prescribed exercise
- Education and training
- Psychosocial assessment
- Goal-based outcomes assessment
- Individualized treatment plan
Source: A Rural Hospital Guide to Improving Chronic Obstructive Pulmonary Disease
"As part of an Accountable Care Organization,
we're concerned about population health,"
Johnson said, sharing that HCMC was poised for an
original start date of January 2020. "Despite
the reimbursement issues, we realized there was no other
reason not to add this program. It's that
important to the overall health of our
community."

Johnson shared that prior to the COVID-19 public health emergency, the organization's chronic care management team had identified nearly 100 potentially eligible patients. The healthcare organization stayed connected with a small percentage of these patients during the past year despite the fact that the PR program has not officially started. He said he realized that some of the COPD patients who first expressed interest in PR were also some of the first community members leading by example when they — because of their lung disease — followed physical distancing suggestions. Though COVID-19 did delay the program's start, Johnson said now that these patients are vaccinated, they are actually requesting PR.
"We've seen that our community's COPD patients were some of the first to get vaccinated and they want to get started on rehab," he said. "We'll be starting shortly and in the way that we had originally envisioned the program. I feel very good about our next steps and now we can really dive in and make an impact."
Johnson said that an important part of their strategic planning around the PR program start-up was also recognizing that chronic lung disease and COPD doesn't respect age.
"This disease does not just attack one age group and it's not just related to smoking," he said. "Especially in rural areas with all sorts of occupational exposures, it can start at different times. Symptoms develop at different times. We need to make sure that all age groups are getting their yearly exams and we're identifying people with these lung conditions or at risk for the conditions early."
He said the COVID-19 pandemic has also further energized the team in advance of their upcoming official start.
"Over the last few months, we've accomplished a lot here in rural Nebraska," he said. "We feel even more confident about what our PR program will accomplish for our patients. Our PR program is the story that can be made every day in rural communities. When you're rural, sometimes you think, 'Well, we just don't have the resources to do that.' You'd be surprised about what you can accomplish — and this pandemic has made us realize that we can do just about anything."
Population Health, Pulmonary Rehabilitation, and Rural Michigan

Like Nebraska's Johnson, Steve Barnett, president and CEO of McKenzie Health System (MHS) in rural Michigan, said attending to local population health needs should be considered an important strategy for healthcare organizations hesitant to start a new PR program because of current reimbursement issues.
"These folks with chronic heart and lung problems? Those are the diagnoses at the top when it comes to consuming healthcare resources," Barnett said. "We know that we see more COPD patients in rural areas as compared to urban. Anything we can do to improve these patients' health while mitigating admissions and readmissions is important not only for patients, but in keeping our costs down."
Dr. James Sams, a MHS family medicine provider — and a former respiratory therapist — is the MHS program's medical director and physician champion. He explained that although a Michigan foundation helped with equipment start-up costs, the program, which started in November 2019, had a very modest start in a very small space. Despite its "humble" beginnings, the program saw immediate success.

"As a respiratory therapist and as a medical student and resident, I'd worked in large medical facilities with cardiopulmonary rehab units that looked like NASA space labs," Sams said. "I'd be happy to compare our outcomes with theirs. It's not all about a fancy space and the bells and the whistles. It's about making our patients feel at home and improving their well-being. Our original small space has not deterred success."
Also a respiratory therapist — turned nurse anesthetist — turned hospital administrator, Barnett, along with Sams, the respiratory therapist-now-physician, explained that their prior professional walk in the respiratory therapy space probably lessened their sense of risk that other leaders of start-up PR programs might experience. Yet, despite their full understanding of PR benefits, they both admitted they were surprised at the quick wins their local PR program gained having only started in November 2019. Sams said they've moved from a space they affectionately referred to as a broom closet into a bigger space a few months ago.
Barnett and Sams also explained that despite COVID interruptions, the new program only paused for several months. During those months, they credit the program's continued success to key PR staff who maintained phone connection with enrolled patients. Though no formal telehealth program was used, patients used peak flow meters and were coached on continued home exercise and breathing training.
Now MHS is realizing that the PR program's physical space may need to expand again since so many of the patients who've completed the program are paying a nominal fee for maintenance.

"When we first started this program, many patients came in their wheelchairs," Sams said. "Now they push wheelchairs or push others in wheelchairs. Sometimes they're actually competitive with their new mobility gains. They are so happy with how they feel and they don't want to lose ground. They want to stay with the routine."
Sams said he's heard how grateful patients are with their improved quality of life — due to participation in a program offered right in their home area. He said that some of these patients have actually become great ambassadors not just for pulmonary rehab, but for the health system in general.
"I heard this story where one person told another, 'Hey, my friend from four counties over comes to rehab here. He said it's really good,'" Sams said. "And another responds with, 'I didn't know they even had that at this hospital.' Stories like that open up our doors here, stir up a little bit of pride for our staff as well as our community's pride in our facilities. More people then will stay local for their healthcare."
Barnett said he agrees with Sams that there is no better endorsement than a grateful community's word of mouth about their local healthcare organization.
"You know how difficult it is to describe culture," he said. "But I think a way to describe what we do here with pulmonary rehab and our other services is in contrast to other organizations: We don't deliver care to make profits. We use our profits to deliver care. And it's really just that simple."
More Information
Learn more about pulmonary rehabilitation in this short animated video created by the National Heart, Lung, and Blood Institute, part of the National Institutes of Health.
Pulmonary Rehabilitation: Three Dismal
Facts
- Only
accessed by about 4% of Medicare beneficiaries
with COPD
- Possibly related to PR's "opt in" versus cardiac rehabilitation model of "opt out"
-
Provider nescience
- While nearly 70% of primary care physicians were aware of PR availability, only 40% routinely prescribed it
- Reimbursement disparity compared with cardiac rehabilitation (CR)

