Rural Hunger and Access to Healthy Food
Agricultural production abounds in rural areas, creating an engine for economic growth and opportunity in communities across the U.S. However, gaining access to healthy and affordable food can be a challenge for rural residents. Many rural areas lack food retailers and have limited supplies of fresh, affordable foods, even in areas where farming is important to the local economy.
In rural areas, access to food may be limited by financial constraints, transportation challenges, or a lack of grocery stores. Rural shoppers may be forced to rely on more expensive and less nutritious food, such as the types available at gas station convenience stores or face a long drive to a town with a supermarket or grocery store that stocks fresh produce and other staples.
Some rural residents and households are food insecure, meaning they cannot rely on access to sufficient, affordable, and nutritious food at all times, increasing the risk of poor health outcomes. According to the 2017 United States Department of Agriculture Economic Research Service (USDA-ERS) publication Food Insecurity, Chronic Disease, and Health Among Working-Age Adults, food insecurity is strongly associated with chronic disease and poor health, both of which disproportionately affect rural populations. Long-term food insecurity can affect physical and mental health, development, learning, productivity, and family well-being.
Food security can also be seen as a community-level issue. A 2002 USDA-ERS publication defines the ongoing importance of community food security, which:
“…concerns the underlying social, economic, and institutional factors within a community that affect the quantity and quality of available food and its affordability or price relative to the sufficiency of financial resources available to acquire it.”
This topic guide provides information for healthcare providers, human service providers, and organizations concerned with food security in rural communities. The guide covers:
- How to learn about rural food security in your community
- Strategies rural communities and healthcare providers can use to address rural hunger
- Funding and assistance programs to address food access and nutrition
Frequently Asked Questions
- Why do food deserts exist in rural areas?
- How does food insecurity in rural areas compare to the nation as a whole?
- How does rural food insecurity affect health outcomes?
- How can we assess the level of food security and availability of healthy food in our rural community?
- What strategies have rural communities used to improve access to healthy and affordable food?
- How can rural healthcare organizations address food and nutrition issues in their community?
- How widely used are federal nutrition programs among rural families?
- What nutrition programs are available for children in rural schools, daycare centers, and other settings?
- What food assistance programs are available for seniors in rural communities?
- What are some funding opportunities for rural community food pantries?
Why do food deserts exist in rural areas?
Characteristics and Influential Factors of Food Deserts, from the USDA-ERS, reports that food deserts tend to have smaller populations, higher numbers of vacant homes, higher rates of unemployment, and more residents with lower levels of education and lower incomes.
Many rural areas lack a population base large enough to support a grocery store that stocks a variety of affordable and healthy food, particularly if some residents bypass the local store to shop at distant supermarkets offering lower prices or order groceries online. A 2009 article in the American Journal of Preventive Medicine discusses the economics of rural food access:
“…small town food stores, with limited floor space, economies of scale, and distance from distribution centers, continue to provide limited food selection at higher prices and face the persistent challenge to remain profitable… As a result, rural families with only convenience or small stores from which to choose experience higher prices and lower selection and quality of foods than those shopping in larger supermarkets.”
This issue of limited selection and high prices continues to be an issue for rural communities when their local, independent grocery stores struggle with financial viability.
The 2021 article Quantifying the Food and Physical Activity Environments in Rural, High Obesity Communities discusses how local grocery stores typically have food options with more nutritional value than convenience stores, but because of low population and shifting economies in rural areas, local grocery stores are not always sustainable or able to offer affordable prices for merchandise because of low volume of sales. Additionally, rural residents may struggle to locate options for dining outside the home. According to 2023 article The Rural Food-Away-from-Home Landscape, 1990-2019, rural counties also have fewer food-away-from-home (FAFH) opportunities, with 20% of nonmetro counties having fewer than 10 FAFH options that largely consist of chain restaurants, therefore limiting the quality and diversity of food options for rural residents. With decreasing opportunities to patronize grocery stores or utilize FAFH options, limited food access becomes an issue for rural communities.
How does food insecurity in rural areas compare to the nation as a whole?
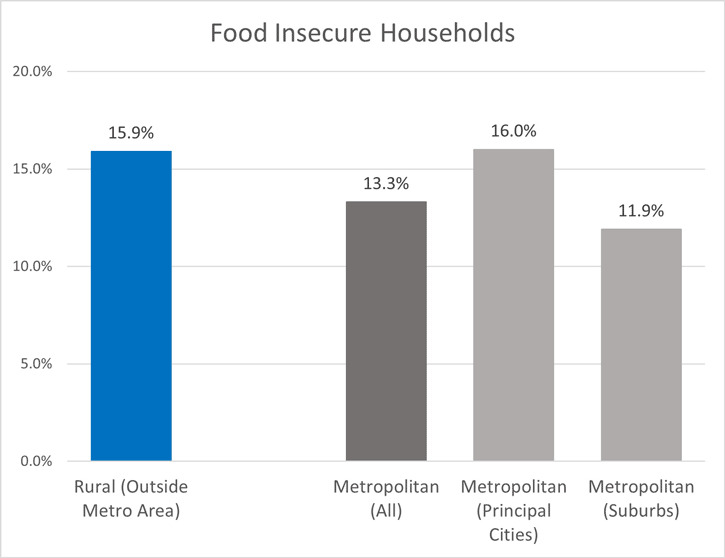
Food insecurity impacts various geographic locations in the United States differently, with rural areas experiencing rising difficulties due to food deserts, lack of transportation, and limited food options. In 2024, 13.7% of U.S. households were food insecure at some time, up from 13.5% in 2023, according to the USDA-ERS report, Household Food Security in the United States in 2024. The same report notes that the rate of food insecurity in rural areas increased, from 15.4% in 2023 to 15.9% in 2024.
Children experience an increased burden related to food insecurity. According to Children Living in Households That Experienced Food Insecurity: United States, 2019-2020, 12.9% of children in nonmetropolitan areas live in a food insecure household. Child Hunger in Rural America reports that 84% of counties in the U.S. that experience the highest levels of childhood food insecurity are rural.
The USDA-ERS also reports that households in rural areas accounted for 15.9% of all food-insecure households in 2023. Severe food insecurity continues to be an issue, with Prevalence of Very Low Food Security, 2022 and 2023 reporting that very low food security worsened between 2022 and 2023 in residences outside of metropolitan areas.
According to Adults Living in Families Experiencing Food Insecurity in the Past 30 Days: United States, 2021, nonmetro adults were the most likely to live in families experiencing food insecurity at 7.7%, compared to 5.8% for medium/small metro, 4.2% for large fringe metro, and 6.4% for large central metro. A 2024 USDA Economic Research Service report states that households outside of metro areas have the highest prevalence of food insecurity at 12.6%, compared to 10.8% of households inside metro areas that experience food insecurity.
How does rural food insecurity affect health outcomes?
Research shows that access to nutritious and affordable food for rural residents is important for improving health behaviors and status. Chapter 8 of the National Research Council's Research Opportunities Concerning the Causes and Consequences of Child Food Insecurity and Hunger: Workshop Summary discusses the literature related to the health of children and pregnant women. It shows that food insecurity and hunger adversely affect child development and academic performance and may contribute to behavioral health disorders, compromised immune systems, and other health issues.
According to the report Patterns of Food Insecurity, Food Availability, and Health Outcomes among Rural and Urban Counties, the risk of food insecurity increases as counties become more rural. The highest food insecurity was found in rural areas of the East South Central census division. Results of the study show significant associations between food insecurity risk and the following:
- Diabetes
- Obesity
- No leisure time physical activity
- Consuming fewer than five servings per day of fruits and vegetables
- Smoking
Food insecure households have limited access to fresh, healthful foods and may purchase less nutritious convenience foods, such as processed, high fat, and high sugar foods, which can cause negative health outcomes. According to Factors Associated with Sugar-Sweetened Beverage Intake Among Young Children – United States, 2021, high sugar intake during childhood from foods such as sugar-sweetened beverages (SSBs) increases the risks for obesity, type 2 diabetes, oral health issues, cardiovascular disease, and asthma, and low-income families, parents with less education, and households living in nonmetropolitan areas are all at higher risk for unhealthy SSB intake. Food Insecurity in the Rural United States: An Examination of Struggles and Coping Mechanisms to Feed a Family among Households with a Low-Income discusses how healthy food is less accessible in rural communities, particularly those with significant poverty. Participants in this study expressed a desire to provide an "ideal meal" for their households that contained proteins, grains, and vegetables, though they struggled to obtain these foods due to issues such as time, availability, transportation, and affordability.
How can we assess the level of food security and availability of healthy food in our rural community?
The Community Food Security Assessment Toolkit was developed by the USDA-ERS to help local government officials, local organizations, and community planners promote food security in all households. The toolkit examines 6 components of community food security:
- Community socioeconomic and demographic characteristics
- Community food resources
- Household food security
- Access to food
- Food availability and affordability
- Community food production resources
Feeding America conducts Map the Meal Gap, a research study represented through an interactive map outlining hunger at the county level. Food insecurity data can be viewed by state, county, food bank service area, and congressional district.
The USDA-ERS Food Access Research Atlas provides information on food access by census tract. This mapping tool uses the following indicators:
- Distance to a store with healthy food or the number of stores in an area
- Low vehicle access areas
- Low-income areas
- Areas in which 67% or more of the population live in group quarters, such as correctional facilities or skilled nursing facilities.
The USDA-ERS Food Environment Atlas provides county-level data on a wider set of statistics regarding food choices, health, and community characteristics. The Food Environment Atlas has maps showing the following factors, all of which influence the diet quality of individuals and communities:
- Access and proximity to a grocery store
- Store availability
- Restaurant availability
- Food assistance
- State food insecurity
- Food prices and taxes
- Local foods
- Health and physical activity
- Socioeconomic characteristics
What strategies have rural communities used to improve access to healthy and affordable food?
Many different approaches have been used to address this issue. The Healthy Food Access Portal can help communities find funding and resources related to retail projects and policy efforts. Strategies include:
Special Financing for Food Retailers
Some rural communities offer subsidized financing for food retailers by participating in state programs. The USDA's Healthy Food Financing Initiative provides capital and technical assistance directly to food retailers and food enterprises who serve rural and underserved communities across the country. The 2023 article Changes in Policy Supports for Healthy Food Retailers, Farmers Markets, and Breastfeeding Among US Municipalities, 2014-2021: National Survey of Community-Based Policy and Environmental Supports for Healthy Eating and Active Living (CBS-HEAL) details additional policies and special financing options that promote healthy food access.
Cooperative Grocery Stores
Some rural grocery stores are community-owned or use the cooperative model. Co-ops have long existed in rural communities to provide key services such as electricity and phone service, where distance and low volumes make providing that service unattractive and unsustainable for traditional businesses.
Cooperatives are composed of members who are both customers and owners. The community-owned model closely resembles the cooperative model, although it is typically organized as a corporation, in which community members can buy shares.
Farmers Markets
Farmers markets can be established in rural areas to help small local farmers financially, while also increasing access to fresh fruits and vegetables for local residents. However, it can be a challenge to establish a rural farmers market, due to large geographic distances and the small number of potential shoppers. Farmers' Market Challenges in a Rural Setting: A Case Study of the Elaney Wood Heritage Farmers Market explores strategies of a rural North Carolina farmers market for attracting and retaining vendors and customers. Rural Farmers Market Promotes Food Security highlights how one farmers market in rural Michigan has promoted programs to help residents access fresh produce more easily.
The Supplemental Nutrition Assistance Program (SNAP) and the Special Supplemental Nutrition Program for Women, Infants and Children (WIC) encourage farmers markets to accept their program benefits. Working With Rural Producers to Expand EBT in Farmers' Markets: A Case Study in Hardeman County, Tennessee discusses an Extension program that encouraged rural producers to accept SNAP benefits through Electronic Benefit Transfer (EBT) and advertise at farmers markets.
Community Supported Agriculture Programs
In community supported agriculture programs (CSAs), local residents commit to purchasing part of a local farmer's crop at the beginning of the year. Farmers receive a cash investment to operate their farm and residents receive a supply of fresh produce. This program allows farmers and consumers to share the risks and benefits of local farming.
Farm to School Initiatives
Farm to school initiatives help local farmers sell fresh fruits and vegetables directly to public schools or incorporate school gardens in meal programs so that nutritious meals and snacks can be served to students and teachers, as well as educating children about nutrition and local farming. The Center for Integrated Agricultural Systems offers toolkits and other resources related to farm to school initiatives. Our Rural Schools and Health topic guide has more information about how schools can provide access to nutritious meals for students.
Food Pantries
Food pantries and other forms of direct food assistance, such as backpack food programs for children, can fill an important need for rural residents experiencing food insecurity. Food pantries can distribute nutritious food to low-income families and work with the local social services staff to give families information on nutrition, the Supplemental Nutrition Assistance Program (SNAP), and other social services in the community. Mobile food pantry trucks may be an option in rural communities without a suitable place to store and distribute food. For example, the Care and Share Food Bank provides mobile food pantry services to rural communities across Southern Colorado.
Collaboration with Public Libraries
Some communities collaborate with public libraries to offer food pantry provisions or lunches during the summer months. Public libraries were particularly helpful for food distribution during the COVID-19 pandemic, and some communities chose to make funding permanent for these programs going forward. See Serving Up Solutions: Innovative Approaches to Delivering Non-Congregate Summer Meals in Rural Areas for an example of a summer meal program from the California Library Association.
Community Education and Outreach
Community programs that improve access to food may also include education and outreach activities. Approaches to assist low-income residents include education on food assistance programs, social services, and training related to home economics, such as cooking from scratch and shopping wisely. In addition, community organizations can plant community gardens and teach people how to grow their own food.
Accessible community transportation can also improve food security. Public Transit Supports for Food Access: 2021 National Survey of Community-Based Policy and Environmental Supports for Healthy Eating and Active Living (CBS HEAL) discusses the importance of public transportation and transit planning to promote food access.
How can rural healthcare organizations address food and nutrition issues in their community?
Rural healthcare organizations can work with human services providers to ensure that low-income patients are able to access healthy food options. Human services organizations may be able to offer training and tools to primary care providers so that they can screen patients for food insecurity. Addressing Food Insecurity in Health Care Settings provides tips for screening patients for food insecurity and providing interventions, such as referrals. Healthcare providers can refer patients to:
- Local food pantries
- Human services agencies for food assistance programs
- Women, Infants, and Children (WIC) offices
- Meal programs for seniors
In addition, rural healthcare providers can provide counseling and nutrition education for patients to promote wellness and help manage chronic disease. Facilities may partner with other community organizations and businesses to provide or refer patients to cooking classes, meal programs, and other nutrition-related services and education.
Healthcare providers can also prescribe healthy foods. Providing Patients with Access to Nutritious Food describes programs in which medical facilities actively promote consumption of healthy foods among patients and local residents. The Lakewood Health System, in rural Minnesota, created Lakewood Engage, a program designed to improve access to safe, nutritious, and affordable food for positive health impact. See Development and Evaluation of the Delivery-Based HEALED Produce Rx Program for Uninsured Patients With Diabetes in Rural Eastern North Carolina as well as Produce Prescription Programs Offer 'A Holistic Approach' to Addressing Rural Food Insecurity and Diet-Related Disease for more examples of produce prescription programs in rural areas. Additionally, the Models and Innovations section of this topic guide provides more examples of projects conducted in rural communities.
How widely used are federal nutrition programs among rural families?
The USDA Food and Nutrition Service's Supplemental Nutrition Assistance Program (SNAP) helps low-income individuals and families buy nutritious food. According to the USDA-ERS report, Alleviating Poverty in the United States: The Critical Role of SNAP Benefits, rural areas have higher rates of poverty and higher use of SNAP benefits than metropolitan areas. Furthermore, child poverty is higher in rural areas. One of the report's key findings is that SNAP benefits are particularly effective in reducing poverty for people in nonmetropolitan areas.
The October 2024 document Trends in Supplemental Nutrition Assistance Program Participation Rates: Fiscal Year 2020 to Fiscal Year 2022 reports that in FY 2022 there was a 94.2% participation rate among SNAP-eligible people in rural areas, and an 86.4% rate among their urban counterparts. According to Characteristics of Supplemental Nutrition Assistance Program Households: Fiscal Year 2022, 15.9% of all SNAP households are in micropolitan or non-core rural areas.
The USDA Food and Nutrition Service’s Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) serves low-income women, infants, and children up to age five who are at nutritional risk. WIC provides nutritious food, information on healthy eating, education on breastfeeding, and referrals to healthcare. According to the Food Research & Action Center's 2018 document Rural Hunger in America, the percentage of income-eligible families with young children participating in the WIC program is higher in rural areas (46%) than in metropolitan areas (42%).
What nutrition programs are available for children in rural schools, daycare centers, and other settings?
In addition to SNAP, nutrition programs available for rural children include:
- School Breakfast Program
- National School Lunch Program
- Special Milk Program
- Child and Adult Care Food Program: Afterschool Program
- SUN Meals (Summer Food Service Program)
The Summer Meals Site Finder helps locate free summer meals for kids within a 15-mile radius. For more information on school nutrition programs, see our Rural Schools and Health topic guide.
The Child and Adult Care Food Program (CACFP) provides financial assistance to childcare centers for nutritious meals and snacks. The program helps in-home daycare providers, daycare centers, afterschool programs, and emergency shelters improve access to healthy food. Their website also provides nutrition education, healthy recipes, and wellness resources.
One barrier for eligible rural families to participate in the Child and Adult Care Food Program is that rural children are more likely to receive care in a relative's home than in a daycare center or afterschool program which qualifies for the Child and Adult Care Food Program. Other challenges to increasing enrollment in child nutrition programs for eligible rural families include a lack of awareness about existing programs as well as a stigma related to receiving government assistance. Rural families may also have a more difficult time utilizing the SUN Meals (Summer Food Service Program) because of the distance needed to travel to a participating site. One example of a community addressing this issue comes from Blaine County, Idaho, where The Hunger Coalition's Bloom Truck and Bloom Markets provide healthy sack lunches to children in the summer. For more strategies related to addressing childhood hunger, see No Kid Hungry's Center for Best Practices repository of tools and resources.
What food assistance programs are available for seniors in rural communities?
Food insecurity has a significant impact on rural seniors. According to Food Insecurity Among Seniors and Older Adults in 2022, 10.2% of seniors in nonmetro areas are food insecure, compared to 8.5% in metro areas. Nutrition Services programs funded through the Administration on Aging provide access to nutritious meals, education, and nutrition counseling for adults ages 60 and above, particularly those who have social and economic need. Programs vary depending on the needs and the resources available in each community.
Congregate meal programs offer meals in a central setting, such as a senior center. Home-delivered meal programs, such as Meals on Wheels, bring meals to the homes of frail, homebound, or isolated older adults. Providing hot home-delivered meals to older adults living in remote rural communities can be a challenge due to travel distance and time required for delivery. In some locations, frozen meals or sack lunches can be delivered on a less frequent basis or picked up from a designated location. Often there is a suggested donation or sliding fee schedule to defray the cost of meals. For more information, see the 2023 Meals on Wheels and Rural Communities, with Carter Florence and Shon Gress episode of the Exploring Rural Health podcast.
The Child and Adult Care Food Program (CACFP) is a federal program that provides healthy meals and snacks to adults receiving day care. Adult daycare centers receive payments for serving healthy meals to adults who are 60 or older, or who are physically or mentally impaired to a degree that limits their independence.
The Senior Farmers' Market Nutrition Program (SFMNP) is offered through the USDA Food and Nutrition Service to provide low-income seniors with coupons that can be used at farmers markets, roadside food stands, and community-supported agriculture programs to promote the consumption of fresh fruits and vegetables among seniors.
The Commodity Supplemental Food Program works to improve the health of low-income people at least 60 years of age by distributing shelf-stable food and administrative funds to participating states and tribal organizations.
USAging has more information about home and community-based services available to seniors.
What are some funding opportunities for rural community food pantries?
To set up a food pantry in a rural community, it is helpful to start by contacting your local Feeding America food bank. Food banks provide a range of supports and expertise for launching and maintaining an effective food pantry, and collectively, the Feeding America network serves every county in the United States allowing for a culture of learning and sharing best practices for rural, urban, and suburban communities alike.
Rural food pantries may receive donations from many sources, including federal programs, state government, foundations, corporations, churches, and individuals.
The Emergency Food Assistance Program (TEFAP) is a federal program that makes food available to State Distributing Agencies such as food banks, which then provide food to local pantries and other organizations.
The Rural Health Information Hub has a list of funding opportunities regarding food and hunger. You can also contact us at info@ruralhealthinfo.org or 800.270.1898 for a customized funding search.

