Social Determinants of Health for Rural People
According to Healthy People 2030, the social determinants of health (SDOH), sometimes referred to as social drivers of health, are
“the conditions in the environments where people are born, live, learn, work, play, worship, and age that affect a wide range of health, functioning, and quality-of-life outcomes and risks.”
Income, educational attainment, demographics, health literacy, infrastructure, and environmental factors all impact the ability of people to access health and community services to meet their basic needs, such as clean water, nutritious food, and safe housing, which are essential to staying healthy. Rural residents are more likely to experience some of the contributing social factors that impact health, such as poverty and issues of access. The impact of these challenges can be compounded by the barriers already present in rural areas, such as limited public transportation options and fewer choices to acquire healthy food. By focusing on SDOH, communities can greatly improve the population health of their citizens and lessen the burden on their healthcare systems.
This guide focuses on the social determinants of health that rural residents experience, including:
- Income, employment, and poverty
- Educational attainment and literacy
- Environmental health, including water quality, air quality, and pollution
- Access to safe and healthy homes, including issues related to energy costs and weatherization needs, plumbing, lead-based paint, and other safety issues
- Access to safe and affordable transportation
- Access to healthy and affordable food
- Access to human services and medical-legal partnerships
- Adequate community infrastructure, such as telephone and broadband internet access
Two related guides are available to learn about the impacts of the social determinants of health (see Rural Health Disparities) and ways to address them to improve health (see Human Services to Support Rural Healthcare).
Frequently Asked Questions
- What is the Vital Conditions for Health and Well-Being framework?
- How does Rural America differ from the nation as a whole regarding the social determinants of health?
- What is being done to address the social determinants of health for rural residents?
- How do poverty and unemployment impact health in rural communities?
- How does early childhood development act as a social determinant in rural areas? What programs and projects are available to address this?
- What are the roles of educational attainment, literacy, and health literacy, in the health of rural residents?
- What types of environmental hazards do rural communities face that endanger the health of their residents?
- How does the quality of housing available in rural areas impact people's health?
- How does rural homelessness impact health?
- How can a lack of transportation options impact low-income, frail elderly, and disabled rural residents?
- How do rural residents experience food insecurity?
- How do rural residents access human services that help them address social determinants of health?
- What can healthcare providers do to help address the social determinants of health for their patients?
- How can rural medical-legal partnerships help address legal needs that impact health?
- How do telephone services and broadband access impact health?
- How does healthcare access act as a social determinant of health for rural people?
What is the Vital Conditions for Health and Well-Being framework?
There are a variety of definitions that encompass the ideas related to the social determinants of health, including the Seven Vital Conditions for Health and Well-Being Framework. This framework posits that certain conditions must be met, over multiple generations, for populations to experience holistic health and well-being. These vital conditions include:
- Humane housing
- Belonging and civic muscle
- Basic needs for health and safety
- Reliable transportation
- Meaningful work and wealth
- Lifelong learning
- Thriving natural world
How does Rural America differ from the nation as a whole regarding the social determinants of health?
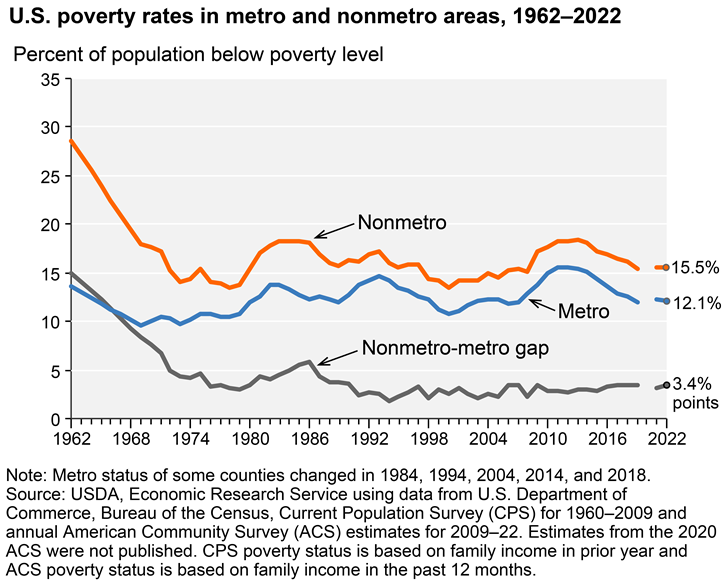
Rural America faces noteworthy challenges related to social determinants of health compared to the nation as a whole. On average, rural residents have fewer individual resources, lower incomes, and less education. This Economic Research Service chart shows the ongoing gap between metropolitan and non-metro poverty rates:
Many rural residents face additional barriers such as access to housing, transportation, food, and water that are safe, healthy, and affordable. These barriers can impact all residents, though they are particularly problematic for those already struggling financially.
Rural communities also face many environmental challenges. Hazardous materials often end up in remote areas where the land is cheap and fewer people overall are put at risk. Rural industries like mining and farming bring with them their own dangers and environmental impacts.
A variety of well-being indexes and tools share data and rankings based on factors that include social determinants of health. Some examples include:
- CDC/ATSDR Social Vulnerability Index, Agency for Toxic Substances and Disease Registry, Centers for Disease Control and Prevention (CDC)
- Community Resilience Estimates, U.S. Census Bureau
- Multidimensional Index of Deep Disadvantage, University of Michigan
- Neighborhood Atlas, University of Wisconsin School of Medicine and Public Health
- The Opportunity Atlas, Brown University, Harvard University, U.S. Census Bureau
- Area Deprivation Index, University of Wisconsin
What is being done to address the social determinants of health for rural residents?
An ever-increasing number of federal agencies, foundations, and health-related organizations are taking an interest in the social determinants of health in general, and many are looking specifically at rural areas.
Just a few of these undertakings include:
- 2015 and 2016 meetings of the National Advisory Committee on Rural Health and Human Services looked at rural poverty and the social determinants of health. The December 2015 NACRHHS policy brief, Child Poverty in Rural America, summarizes their findings from the Minnesota meeting. A January 2017 policy brief, Social Determinants of Health, summarizes their findings from the New Mexico meeting and offers policy recommendations for addressing the social determinants of health in rural communities.
- The U.S. Department of Health and Human Services Office of the Assistant Secretary for Planning and Evaluation issued December 2016 and March 2020 reports to Congress on Medicare's value-based purchasing programs that looked at a variety of social factors that impact health, including rurality.
- The 2022 Assistant Secretary for Planning and Evaluation Office of Health Policy report, Addressing Social Determinants of Health: Examples of Successful Evidence-Based Strategies and Current Federal Efforts, which discusses the importance of upstream interventions to promote positive healthcare outcomes.
How do poverty and unemployment impact health in rural communities?
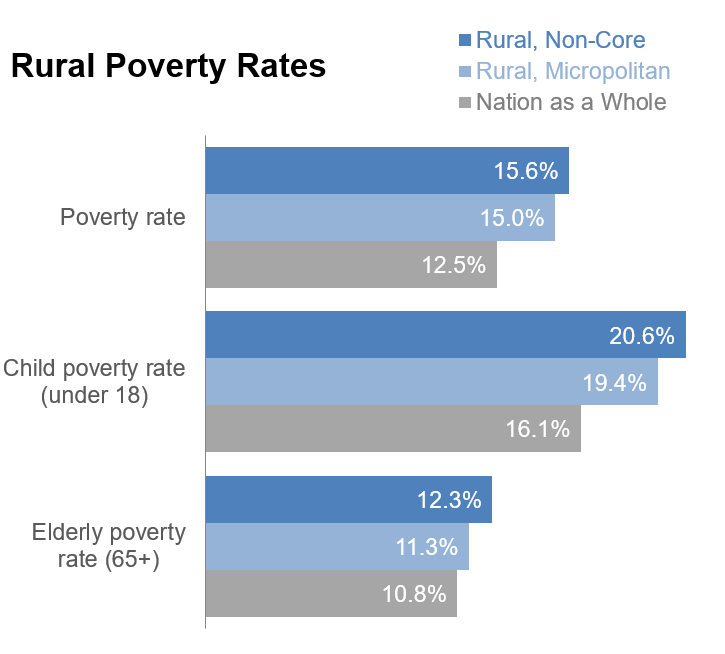
Poverty is an ongoing problem for many rural areas. The 2014 RUPRI publication Persistent Poverty Dynamics: Understanding Poverty Trends Over 50 Years reports on counties with poverty rates above 20% over the past 50 years. Sixty-four percent of non-core (small rural) counties are persistent poverty counties, compared to 22% of micropolitan (large rural) and 14% of metropolitan counties.
Rural areas have higher poverty rates, particularly among children and the elderly:
Average household income is lower in rural areas. According to Income in the United States: 2024, households outside a metropolitan statistical area had an average household income of $63,750, compared to $87,410 for households inside a metropolitan statistical area.
Among the impacts of poverty on health is the barrier it creates in paying for healthcare services and meeting basic living needs, such as food and shelter, that are necessary to be healthy. Poverty also exerts an influence over both physical and mental health due to the stress it causes.
The availability of good jobs — jobs that pay a living wage, offer adequate hours, and include benefits such as health insurance coverage and paid sick leave — can also impact rural residents' ability to stay healthy. According to the 2024 report Changes in the U.S. Economy and Rural-Urban Employment Disparities, low-skill occupations are more common in areas with less population density, while high-skill occupations are more common in metro areas with higher population density. This disparity can impact the quality of job opportunities for rural citizens. Workers in metro areas statistically have higher levels of education compared to those in nonmetro areas, which worsens unemployment levels in rural areas:
| Education Level | Metro Counties | Nonmetro Counties |
|---|---|---|
| Less than high school graduate | 57.2 | 46.2 |
| High school graduate (including equivalency) | 68.5 | 64.2 |
| Some college or associate’s degree | 76.0 | 73.3 |
| Bachelor’s degree or higher | 84.6 | 82.7 |
| Total, population 25 to 64 years | 75.5 | 68.9 |
| Source: Table 5, Changes in the U.S. Economy and Rural-Urban Employment Disparities, Board of Governors of the Federal Reserve System. | ||
In addition, rural workers with a college degree may find they earn less than their counterparts who work in urban areas. However, those with less education may earn higher wages in rural areas:
| Education Level | Rural | Nation as a Whole |
|---|---|---|
| All education levels | $49,962 | $52,696 |
| Less than high school graduate | $34,214 | $32,485 |
| High school graduate | $41,500 | $40,153 |
| Some college or associate's degree | $47,662 | $47,260 |
| Bachelor's degree | $64,499 | $70,044 |
| Graduate or professional degree | $80,086 | $90,720 |
| Source: Table B20004, 2020-2024 American Community Survey 5-Year Estimates | ||
According to a 2023 article, Rural/Urban Differences in Access to Paid Sick Leave Among Full-Time Workers, access to paid sick leave for full-time workers in rural areas was 69.8%, compared to 76.4% for full-time workers in urban areas, after adjusting for other sociodemographic variables. Without access to paid sick leave for themselves or their family members, rural citizens are more likely to work while sick, which can delay necessary treatment, pass contagious diseases on to others, and increase the likelihood of utilizing emergency departments for care.
How does early childhood development act as a social determinant in rural areas? What programs and projects are available to address this?
Early childhood development programs have the potential to impact health at a young age and set children on a path to grow to be healthy adults. According to Healthy People 2030,
“Early childhood development and education are key determinants of future health and well–being. Addressing the disparities in access to early childhood development and education opportunities can greatly bolster young children's future health outcomes.”
The 2023 publication Closing the Opportunity Gap for Young Children states that some children may face poverty, food insecurity, exposure to violence, inadequate healthcare, and poorly funded schools, which in turn negatively impacts physical, emotional, and cognitive development. Rural areas tend to have less access to early childhood programs while also having higher levels of adverse childhood experiences (ACEs), which can lead to poor health outcomes in children.
Prenatal care as a social determinant
Rural areas experience healthcare disparities related to prenatal care. Health Disparities in Rural Women reports on decreasing access to obstetric services in rural areas. More than half of rural women live more than 30 minutes from a hospital offering delivery and nursery services. Rural women also tend to begin prenatal care later than suburban women. A 2020 infographic from the University of Minnesota Rural Health Research Center, Loss of Hospital-based Obstetric Services in Rural Counties in the United States, 2004-2018, demonstrates that the percentage of rural counties with hospital-obstetric services decreased from 82% to 77% in micropolitan counties, and 40% to 27% in noncore counties. Infant mortality is higher in nonmetropolitan counties, with a 2019 rate of 6.4 per 1,000 in nonmetro counties compared to 5.4 in metro counties. According to the 2022 article A Critical Review on the Complex Interplay between Social Determinants of Health and Maternal and Infant Mortality, infant mortality rates are higher in rural areas due to higher levels of risk factors, socioeconomic disadvantage, and unequal access to healthcare. For more information on maternal health issues, see the Rural Maternal Health topic guide.
Child care as a social determinant
Child care access acts as a social determinant of health for two main reasons: 1) the ability for the parents to be employed and earn an income, and 2) the importance of quality child care in terms of early childhood development and education. Without adequate child care, parents may struggle to secure consistent employment for themselves and quality early childhood education for their children. A 2018 Center for American Progress report, America's Child Care Deserts in 2018, found that 59% of rural communities in the United States are classified as childcare deserts, or areas lacking in adequate childcare center spaces for children under age 5. According to a Bipartisan Policy Center (BPC) survey conducted in 2019 by Morning Consult, nearly 62% of families living in rural areas said they had difficulty finding quality child care to fit their budget; however, less than half of families living in urban areas said the same. The 2023 policy brief, Childcare Need and Availability In Rural Areas, provides recommendations for improving childcare provider supply in rural communities, such as supporting opportunities for training, recruitment, and teaching waivers so employees can begin working sooner.
Educational opportunities as a social determinant
Head Start is an early childhood education program that serves families with children through age 5 and provides early learning, health, and well-being services. Rural Head Start programs have difficulty maintaining an adequately trained workforce of early childhood educators, according to a 2012 National Advisory Committee on Rural Health and Human Services policy brief, Challenges to Head Start and Early Childhood Development Programs in Rural Communities. They also face challenges providing the transportation necessary to get rural children to both the preschool and healthcare services required for Head Start. Some Head Start programs are home-based, and use a home visiting model to bring services directly to families, which can be an effective delivery method in rural areas. Rural school-age children and youth also have fewer summer opportunities that support health and learning, as explained in Shaping Summertime Experiences: Opportunities to Promote Healthy Development and Well-Being for Children and Youth, a 2019 National Academies of Sciences, Engineering, and Medicine consensus report.
Some of the early childhood factors identified in the Improving Early Childhood Development: WHO Guideline that positively impact health include:
- Prenatal and delivery care
- Violence and injury prevention
- Responsive caregiving from parents and other direct caregivers
- Early learning opportunities
- Optimal nutrition for infants and young children
- Maternal mental health
Programs that can intervene to address early childhood development include:
- Comprehensive child wellness programs like Project LAUNCH (Linking Actions for Unmet Needs in Children's Health).
- Nutrition programs such as the USDA's Special Supplemental Nutrition Program for Women, Infants, and Children (WIC), which provides food and nutrition education to pregnant and postpartum women, and infants and children through age 5 who would not otherwise have enough nutritious food, and the Child and Adult Care Food Program (CACFP), which helps childcare providers offer high-quality meals to children in daycare and afterschool programs.
- Home visiting programs that promote maternal and child health, child development, and positive parenting, such as those supported by HRSA's Maternal, Infant, and Early Childhood Home Visiting (MIECHV) funding.
- Programs that support full-day, full-year quality childcare, with healthy food, physical activity, appropriate learning opportunities, and role models for healthy emotional and social well-being. For example, Healthy Kids, Healthy Future provides tools for child care and early education providers to help children develop healthy habits.
- Early childhood education programs like Head Start and Early Head Start, which help low-income families and children get ready for school through preschool education, health, and social services.
- Full-service community schools that use a model like the CDC's Whole School, Whole Community, Whole Child (WSCC) approach to help children establish healthy behaviors. For more information, see the Coalition for Community Schools.
For information on how schools can support health, see the Rural Schools and Health topic guide.
Examples of rural projects addressing early childhood development as a social determinant include:
- Healthy Connections, Inc. Healthy Families America (HCI HFA), which provides prenatal check-ups, education, transportation, well-baby checks, and child immunizations.
- MIST: Mothers and Infants Sober Together, which helps rural Tennessee mothers with substance abuse problems provide a safe, drug-free home for themselves and their newborn.
- The Healthy Early Learning Project (HELP), offering physical and nutritional programs to preschools in rural Kansas.
What are the roles of educational attainment, literacy, and health literacy, in the health of rural residents?
Education can have multiple impacts on the health outcomes of an individual. Lower educational attainment impacts median earnings, which is already lower in rural areas on average. This chart from the USDA Economic Research Service shows the relationship of education levels and median earnings for rural adults:
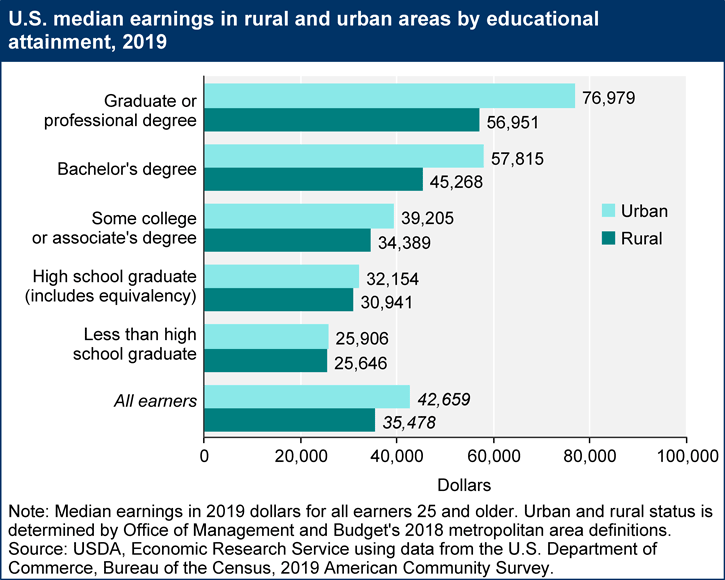
Lower incomes can make it harder to access the already sometimes scarce healthcare resources, educational opportunities, and social services in rural areas. However, income levels are not the only impact that education has on well-being.
Many studies have shown that educational attainment impacts health. A 2006 report from the Organisation for Economic Co-operation and Development (OECD's) Centre for Educational Research and Innovation, Measuring the Effects of Education on Health and Civic Engagement: Proceedings of the Copenhagen Symposium, includes the chapter What Are the Effects of Education on Health? This document reviews the evidence that more years of education result in:
- Healthier behaviors
- Better health outcomes, including birth outcomes
- Higher use of preventive healthcare
- Increased life expectancy
A 2011 Population and Development Review article, The Education Effect on Population Health: A Reassessment, points out that many assume education is merely a stand-in for better socioeconomic status. The authors examined a wide range of studies that looked at education and health, and found that when socioeconomic status was controlled for, the positive impact of education persisted. A 2014 Center on Society and Health issue brief, Health Care: Necessary But Not Sufficient, reports that, for a group of patients with the same access to healthcare via coverage by the same healthcare plan and providers, those with less education had poorer health. Lower levels of education may result in lower overall literacy, impacting a patient's ability to understand and act on health information. A 2004 article in the Journal of General Internal Medicine, Literacy and Health Outcomes: A Systematic Review of the Literature, reports on a review of 44 studies which found poorer health outcomes for those with poor reading skills. Studies reviewed linked low literacy to:
- Less likelihood of having health screenings and prevention services
- Higher risk of hospitalization
- Poorer health status
Health literacy is the degree to which patients understand basic health information such as following instructions from a healthcare provider, managing a chronic illness, or taking medication properly. Rural residents are at risk for low health literacy because they have lower educational levels as compared to residents of metropolitan areas. Low health literacy is a particular problem for people in poverty and people with limited education or English proficiency. According to the book, Health Literacy Interventions and Outcomes: An Updated Systematic Review, limited health literacy is associated with a lower likelihood of using preventive health services, a greater likelihood of taking medicines incorrectly, and poor health status.
The role of education, literacy, and health literacy on health is critical for rural communities, where educational attainment lags behind the nation as a whole.
Rural programs to help students complete high school could have a long-term impact on the health of the rural population. Programs to help adults with low literacy improve their reading skills likewise could have health benefits for participants. Libraries can also help rural communities access healthcare by utilizing librarians as liaisons to help citizens understand healthcare systems and information. See the video, The Rural Library and Health Cooperative Agreement Program: A New Chapter in Rural Healthcare Access, to learn about such a program that is working in rural South Carolina.
Rural public colleges and universities can also provide higher education opportunities in largely rural areas, as well as serving as educational and economic hubs within their regions. Introducing Our Nation's Rural-Serving Postsecondary Institutions Moving Toward Greater Visibility and Appreciation provides information on how rural postsecondary institutions can benefit rural populations.
Some communities are utilizing community health workers to address educational and literacy disparities. See the 2023 publication Engaging Community Health Workers/Youth Ambassadors to Improve Health Literacy: Proceedings of a Workshop – in Brief for more information about improving health literacy in rural areas. Rural providers can also help address health literacy, as shown in these Rural Monitor articles which highlight health literacy tools and resources:
- A New Era of Health Literacy? Expanded Definitions, Digital Influences, and Rural Perspectives
- Rural Health Literacy: Understanding Skills and Demands is Key to Improvement
- Rural Health Literacy: Who's Delivering Health Information?
What types of environmental hazards do rural communities face that endanger the health of their residents?
Many rural areas face substandard water and air quality, along with other environmental challenges. Some of these problems are due to limited infrastructure to support public health, while others relate primarily to the impact of agriculture, logging, mining, and other industries on the environment. Disinvestment in rural communities is another factor that contributes to a higher environmental hazard burden.
Rebuilding the Unity of Health and the Environment in Rural America: Workshop Summary, a 2006 publication from the Institute of Medicine Roundtable on Environmental Health Sciences, Research, and Medicine, identified environmental issues faced by some rural communities, which are all still concerns today. They include:
- Exposure to pesticides, chemicals, and other toxins in ground water
- Air pollution, including dust and soil, pesticides, endotoxins, and other airborne pollutants
- Exposure to disease and animal waste for those working in animal production
These exposures can contribute to poorer health outcomes in rural populations. See the 2023 article, Developing a National-Scale Exposure Index for Combined Environmental Hazards and Social Stressors and Applications to the Environmental Influences on Child Health Outcomes (ECHO) Cohort, for more information on evaluating exposure risk related to issues such as pollution, lack of green space, social economic status, social vulnerability, and more.
Rural Water Quality
A 2015 report from the Government Accountability Office (GAO), Rural Water Infrastructure: Federal Agencies Provide Funding but Could Increase Coordination to Help Communities, reports that rural communities struggle to pay for improvements related to aging and outdated water and wastewater systems. These challenges result from:
- Fewer users of the water system to share the cost of major improvement projects
- Lack of technical expertise, resulting in a need to hire outside consultants to develop a project and complete the documentation required to apply for federal or state assistance
There may be water quality concerns for water systems not covered by the Safe Drinking Water Act, which does not regulate wells serving fewer than 25 individuals. According to U.S. Poison Control’s guidelines on well water safety, rural households relying on private well water or water from very small water systems face dangers from chemical and bacterial contamination. A 2017 Morbidity and Mortality Weekly Report article, Rural and Urban Differences in Air Quality, 2008-2012, and Community Drinking Water Quality, 2010-2015 — United States, reports that water quality decreases from urban to rural areas, based on a study of 10 contaminants.
A 2020 GAO report, Alternative Drinking Water Systems: Use by Very Small Communities, Related Cost Savings, and Technical Assistance Provided by EPA and USDA, identifies cost-effective options for communities of fewer than 10,000 people. Running Clear: Preventing Private Water Sources from Becoming a Health Hazard in Rural America, a June 2019 Rural Monitor article, describes safety concerns for private water sources and how the quality of well water can be ensured.
In addition to the infrastructure challenges, rural water quality may also be impacted by industrial pollution. The Environmental Protection Agency, in a 2015 publication Ground Water Contamination – Getting Up to Speed, identifies the following sources of contamination, all of which may impact rural water quality:
- Waste from active and abandoned mines
- Agricultural sources such as pesticides and manure
- Landfills
- Road salt
- Improperly constructed or abandoned wells
- Underground and aboveground storage tanks
Oil and natural gas production, including hydraulic fracturing (fracking), also can negatively impact rural surface-water and groundwater quality in some circumstances.
A free course, Groundwater and Well Care for Public Water Systems, is available to help owners and operators of non-community water systems learn the basic science of water wells and how to maintain them to ensure safe drinking water.
Rural Air Quality
Outdoor air quality is critical to everyone's health, and is particularly a concern for children, the elderly, people who have underlying health concerns, and those who are frequently outdoors, with health-related impacts of air pollution that include:
- Asthma and other breathing problems
- Pneumonia and bronchitis
- Chronic Obstructive Pulmonary Disease (COPD)
- Heart disease and stroke
- Lung cancer
To learn more about the connection between air quality and health, see the U.S. Environmental Protection Agency’s A Guide to Air Quality and Your Health.
Rural areas face a range of air pollutants caused by:
- Unpaved roads
- Rail transport of hazardous materials
- Pesticides
- Crop harvesting and storage
- Livestock feeding and waste
- Mining, particularly surface mining
- Oil and natural gas drilling
The National Environmental Public Health Tracking Network offers a Data Explorer Tool providing state and county-level data on outdoor air quality indicators.
Examples of rural communities working to address environmental health include:
- The Rural Desert Southwest Brownfields Coalition (RDSBC), a multi-county partnership to clean up brownfields in Nevada and California
- An environmental risk map solution used by the Navajo Nation to limit exposure to uranium in water and soil due to mine-waste contamination
How does the quality of housing available in rural areas impact people's health?
According to a participant from the 2023 policy brief Key Informant Perspectives on Rural Housing and Health,
“We know that there is a direct connection between an individual's health and their physical environment. So when a home is not well maintained, is not well insulated, well heated, well ventilated, where it has had some type of damage, fire or water, or infestation, that hasn't been repaired, there can be a direct correlation between that and the health of the resident.”
While the quality of rural housing has improved in recent decades, there are still pockets of rural America where there is a lack of affordable housing that meets the basic health needs of the population. Taking Stock: Rural People, Rural Places, Rural Housing, a 2023 report from the Housing Assistance Council (HAC), identifies several rural high poverty populations that face particular housing challenges, including farmworkers, tribal communities, and those living in the Lower Mississippi Delta, the rural Southeast, Central Appalachia, or in colonias on the U.S.-Mexico border. According to the report, 5.6% of homes in rural areas of the U.S. are considered inadequate in quality.
Some of the key housing concerns that impact health include:
- Plumbing and wastewater systems (or lack thereof), which can impact water quality and contribute to illness.
- Heating and cooling methods, which impact indoor air quality and safety, for example through the use of kerosene heaters.
- Lack of smoke alarms, carbon dioxide, and carbon monoxide detectors.
- Weatherization needs and energy costs, which impact whether a house can be maintained at a temperature healthy to its inhabitants.
- Safety concerns such as lead-based paint, mold, and pests.
- Overcrowding, which can spread communicable disease and contribute to issues such as substance abuse and domestic violence.
HAC's Taking Stock report identifies a number of concerns related to rural housing quality:
- More than 30% of the nation's housing lacking plumbing is in rural areas, with this burden falling disproportionately on those living in colonias on the U.S.-Mexico border, in tribal communities, in Central Appalachia, the Lower Mississippi Delta, and the rural Southeast.
- Overcrowding is a problem among some low-income rural populations such as farmworkers and can have a particularly negative impact on the well-being of children.
- Rural renters are more likely to live in substandard housing and to experience multiple housing problems related to affordability, quality deficiencies, and crowding, compared to rural homeowners.
The 2022-2023 University of Minnesota Rural Health Research Center project, Housing as a Social Determinant of Rural Health, examines housing issues experienced by rural residents:
- Environmental exposures, such as lead paint, mold, mildew, pests, and air quality
- Less availability of safe cooking equipment and working refrigeration
- Decreased water and sewage quality
- Fewer opportunities for personal wealth and financial stability through property ownership
- Lack of appropriate disability accommodations
The Rural Monitor article Exploring the Intersection of Rural Housing Quality and Health: Healthcare Providers and Housing Experts Provide Insight discusses the impact of rural housing quality on health, as well as how public health and healthcare organizations can work with human services and housing organizations to improve the health and well-being of their community's residents. The Exploring Rural Health podcast episode Rural Housing, featuring David Lipsetz discusses housing issues in rural communities and programs that work to promote safe and affordable housing in rural communities.
For examples of programs to help address rural housing concerns, see What rural housing, energy assistance, and weatherization programs are available? on the Human Services to Support Rural Health topic guide.
How does rural homelessness impact health?
Rural homeless families and individuals face a variety of challenges accessing healthcare. The lack of a stable address can make it difficult to enroll in programs they are eligible for, such as Medicaid. Even when coverage is obtained, rural people who are experiencing homelessness may face challenges finding a healthcare provider. Many need help with mental health and substance abuse problems, and the availability of these services is often limited in rural areas.
Homelessness in Rural America, a 2014 policy brief from the National Advisory Committee on Rural Health and Human Services (NACRHHS), offers an overview of how homelessness impacts rural people. Families with children are a bigger proportion of the homeless population in rural areas, compared to urban areas. A 2019 report from the Institute for Children, Poverty & Homeless, Student Homelessness in Rural America, reports that homelessness among rural public school children is growing at four times the national rate, with an increase of 11% from the 2013-2014 school year to the 2016-2017 school year. The children in families experiencing homelessness are at risk for a range of health-related consequences. According to a 2012 Child Trends publication, When the Bough Breaks: The Effects of Homelessness on Young Children, children who have unstable housing are more likely to experience:
- Emotional and behavioral problems
- Negative impacts on their physical, emotional, and cognitive development
- Hunger
- Missed educational opportunities and poorer academic performance
- Acute and chronic health problems
- Exposure to violence
The NACRHHS brief describes the nature of rural homelessness and the barriers faced by the homeless in rural areas. Rural homeless people are more likely to live in substandard housing, in vehicles, or doubled up with family or friends, rather than on the street. According to America's Rental Housing 2024, only 11% of the rental stock in the U.S. is outside of metro areas, with 48% located in suburban and 40% in urban areas.
Barriers encountered by rural unhoused individuals and families when trying to obtain housing include:
- Difficulty finding transportation to reach services
- A sense of isolation
- Lack of homeless-specific services in their community
- Funding programs that lack the flexibility to meet the particular needs of rural areas
- Lack of employment opportunities to help people become self-sustaining
- Difficulty applying for services, either due to lack of a permanent address or lack of internet access
- Shortages of affordable housing
Since 2010, Pathways Vermont has addressed the homelessness challenge by using an evidence-based, cost-effective housing model, the rural-focused Housing First program, that offers a rapid re-housing program and support services to individuals with mental health and substance use conditions. Pathways also partners with state and community organizations to expand their reach to other populations including families at-risk, veterans, and incarcerated individuals transitioning into society to offset the negative effect of prolonged exposure to homelessness. The Rural Monitor article, Looking at the Rural Homelessness Experience: Definitions, Data, and Solutions, reports on how this approach is helping Vermont's rural homeless population. The Rural Monitor also features other programs aimed at addressing rural homelessness.
How can a lack of transportation options impact low-income, frail elderly, and disabled rural residents?
People living in rural areas tend to be dependent on cars for transportation. These regions often lack the types of public transportation available in more populous areas. Even if there is some form of bus service, it is less likely to run at convenient times for getting to a job, taking children to daycare, or accessing needed healthcare. Of workers 16 and over who live in rural areas, only 0.31% traveled to work by public (non-taxi) transportation, compared to 3.21% for the U.S. as a whole, based on 2020-2024 American Community Survey data (Table B08141).
Low-income rural residents who are fortunate enough to own a vehicle may find the costs of gas and maintenance make it difficult to maintain reliable transportation. Poor rural residents' vehicles are often older and unreliable, and rural drivers are likely to be driving longer distances on secondary roads. Depending on the region, weather and industry may also impact road safety. These factors contribute to the higher risk of traffic injury and death for rural residents.
For those who are not able to drive due to physical limitations, lack of transportation options in rural areas can make it difficult to get to the grocery store and pharmacy, take advantage of social interactions that support good mental health, and access healthcare services. In the Exploring Rural Health podcast episode, Supporting People with Disabilities in Rural Communities, with Rayna Sage and Catherine Ipsen, creative options for transportation such as voucher programs and school bus usage are discussed.
For more information on the impact of transportation on health, see the Transportation to Support Rural Healthcare guide.
How do rural residents experience food insecurity?
Many rural residents have fewer choices to buy fresh and affordable food, making it difficult for them to purchase the nutritious food needed to stay healthy. For those on limited incomes and with limited transportation options, it is even more difficult to meet nutritional needs. According to the USDA Economic Research Service report, Household Food Security in the United States in 2024, 15.9% of rural households are food insecure — lacking access to sufficient food — compared to 13.7% for the nation as a whole. Households with children are impacted even more, with 21.7% of rural households with children being food insecure, compared to 18.4% overall.
Food insecurity is also related to obesity, and obesity levels in rural areas tend to be higher. Rural Healthy People 2020: A Companion Document to Healthy People 2020, Volume 1 looks at rural food insecurity, obesity, and related health problems in the chapter "Nutrition and Weight Status in Rural Areas."
For an in-depth examination of these issues, see the Rural Hunger and Access to Healthy Food and Rural Obesity and Weight Control topic guides.
How do rural residents access human services that help them address social determinants of health?
A range of federal and state programs address human needs, from income supports to job training to housing assistance and more. For detailed information on services available in rural communities, see the following topic guides:
- Human Services to Support Rural Healthcare
- Rural Hunger and Access to Healthy Food
- Transportation to Support Rural Healthcare
The NACRHHS policy brief, The Intersection of Rural Poverty and Federal Human Services Programs, features case studies of two communities using strategies to integrate services to make it easier for people experiencing poverty to access the range of services they need. The Rural Services Integration Toolkit is a guide to developing programs that integrate rural health and human services to better meet rural residents' needs. The toolkit identifies 9 programs in a variety of settings and regions that are taking different approaches to services integration.
State human service agencies provide varying degrees of access to services and to assistance programs via online portals. When available, together with adequate broadband service and other necessary infrastructure, access to human services is faster and easier. Some agencies also offer mobile van services to rural residents, which is a creative strategy that has helped specific populations such as migrant workers. You can find your state agency/agencies in the State Human Services Agencies directory.
For more examples of utilizing human services to improve health outcomes in rural areas, please see Human services in Rural Health Models and Innovations.
What can healthcare providers do to help address the social determinants of health for their patients?
An April 2018 Rural Monitor article, Social Determinants of Health: Transforming the Buzz Phrase to a Rural Action Item, looks at the social determinants from a provider's perspective, discussing what rural healthcare facilities can do to help their patients:
- Tift Regional Health System in rural Georgia conducts social risk assessments for clinic and hospital patients, with support from the CMS Innovation Center's Accountable Health Communities Model.
- CommWell Health's NC-Rurally Engaging and Assisting Clients who are HIV positive and Homeless (NC-REACH) works with community service organizations in rural North Carolina to address housing needs identified through their social determinant risk screening process.
The American Hospital Association (AHA), in an invited commentary in the September 2018 issue of Academic Medicine — Ensuring Access to Quality Health Care in Vulnerable Communities — identifies "addressing social determinants of health" as an important strategy for hospitals. Providers can screen for health-related social needs, help patients access community services, and align local services with patient needs.
In some educational tracks, SDOH are being integrated into the medical curriculum. The 2022 article Integration of Case-Based Dialogue to Enhance Medical Students' Understanding of Using Health Communication to Address Social Determinants of Health discusses teaching third year medical students about SDOH, enhancing their ability to work with various populations as well as rural patients.
Healthcare providers and health systems may want to consult the Commonwealth Fund’s Return on Investment (ROI) Calculator for Partnerships to Address the Social Determinants of Health when considering interventions to address the SDOH. It can help organizations plan sustainable financial arrangements, with a focus on addressing the needs of high-need, high-cost patients.
The Agency for Healthcare Research and Quality offers a guide to help primary care practices collect social needs information from patients and connect them to relevant community resources: Identifying and Addressing Social Needs in Primary Care Settings. Community health needs assessments (CHNAs) can help healthcare organizations determine which social determinants of health would be most impactful to address in their communities. For more on needs assessments, see the Conducting Rural Health Research, Needs Assessments, and Program Evaluations topic guide.
How can rural medical-legal partnerships help address legal needs that impact health?
An April 2022 study from the Legal Services Corporation, The Justice Gap: The Unmet Civil Legal Needs of Low-income Americans, reports on legal needs related to healthcare access, the impact of COVID-19 on American families, and other issues that influence health, such as housing and poverty. It includes an infographic highlighting the prevalence of civil legal problems and the need for legal help for people in rural areas. Rural Legal Deserts Are a Critical Health Determinant discusses how the absence of available attorney services in rural areas exacerbates the SDOH.
Medical-legal partnerships (MLPs) help healthcare providers and lawyers work together in addressing patients' health-harming legal needs. The National Center for Medical-Legal Partnership's How Legal Services Help Health Care Address Social Needs, identifies the following issues where legal aid interventions can help:
- Appealing denial of benefits, such as health insurance, disability benefits, and food stamps
- Addressing housing quality, housing subsidies, and access to utilities
- Protecting workers from discrimination
- Helping veterans with discharge status
- Managing family law concerns related to domestic violence, custody, and other issues
Bringing Law and Medicine Together to Help Rural Patients, an October 2016 Rural Monitor article, highlights rural medical-legal partnerships, and discusses the benefits MLPs bring to rural patients, including:
- Reduced stress levels
- Greater patient engagement
- Improved health outcomes
FirstHealth of the Carolinas, in response to findings from a community health needs assessment, established an MLP in rural North Carolina in partnership with Legal Aid of North Carolina, Inc. Their work is featured in a 2017 Rural Health Value profile, Medical-Legal Partnership Addresses Social Determinants of Health.
How do telephone services and broadband access impact health?
The ability to stay connected to one's friends, family, human services, and healthcare providers is essential for health and well-being. Access to basic telephone service and smartphone technology helps ensure that rural residents can:
- Make appointments with healthcare providers and other service providers
- Contact emergency medical services
- Receive health coaching and other disease management services available by phone
- Stay in touch with family and friends, which may allow rural older adults to stay independent longer and avoid social isolation
A lack of access to smartphone technology and broadband internet is an issue that often overlaps with socioeconomic challenges and a lack of access to healthcare. Connectivity now plays a much greater role in healthcare, with broadband access offering the potential for rural residents to:
- Learn about health topics online
- Access their electronic health records
- Participate in home monitoring and other telehealth services
- Have face-to-face connections with distant family and friends
- Learn about and access government programs
Despite the promise of this technology, not all families are in a position to take advantage of these opportunities. According to the Pew Research Center's August 2021 article, Some Digital Divides Persist Between Rural, Urban and Suburban America, only 72% of rural households have home broadband access, compared to 77% of urban and 79% of suburban households. Mapping Broadband Health in America, a visualization tool from the Federal Communications Commission (FCC), shows broadband access as it relates to health factors and demographics and includes rural data.
In many rural communities, the local library provides access to public computers and the internet, as well as training on how to search for health and other information. Rural Libraries in the United States: Recent Strides, Future, Possibilities, and Meeting Community Needs, a 2017 report from the American Library Association, documents the availability of different services, finding that rural libraries typically offer slower broadband than their urban counterparts but are just as likely as urban libraries to provide public Wi-Fi.
The Federal Communications Commission's Lifeline Program can help make telephone service more affordable for low-income people. To better meet the expanding need for connectivity, in March 2016 the program was expanded to also support discounted broadband for those who qualify. The FCC's Connect America Fund (CAF) aims to accelerate infrastructure development by subsidizing telephone companies to add broadband service where it is not yet available, including rural areas. Connecting Americans to Health Care is an FCC initiative supporting telehealth focused on the potential of remote patient monitoring and mobile health applications to help rural patients.
How does healthcare access act as a social determinant of health for rural people?
Social determinants that impact access to healthcare include:
-
Poverty, income, and employment status, all of which contribute to whether an individual has:
- Health insurance coverage, whether through an employer, a public program, or their own purchase
- The ability to pay out-of-pocket costs such as co-pays and prescription drug costs
- Access to dental care, either through dental insurance or the ability to pay for treatment
- Time off work to go to an appointment
- Resources to afford retirement and pay for healthcare and health-related expenses in retirement, including costs related to aging in place
- The health literacy skills to effectively communicate with healthcare providers and self-manage care
- A means of transportation to visit a healthcare provider
- Smartphone technology and broadband access to utilize telehealth services
Healthcare access can itself act as a social determinant for rural residents. Living in a rural community that has limited health services available is an added barrier to achieving good health. The burden may be a lack of a specific kind of service, such as dental or behavioral health services, or may be related to the hours that a service is available, for example weekends and evenings. A June 2016 issue brief, Impacts of the Affordable Care Act's Medicaid Expansion on Insurance Coverage and Access to Care, found that increased healthcare access through Medicaid expansion improved individuals' financial well-being.
Certain public health services, which support population health, may also be less available in rural communities. For example, rural residents have less access to fluoridated water. While this is partly because they are more likely to be on well water, rural water systems are also less likely to be fluoridated. For more information on fluoridation, see Where can I find information about fluoridation in rural community water supplies? on the Oral Health in Rural Communities topic guide. For additional information on rural public health services, see the Rural Public Health Agencies topic guide.
A lack of healthcare and public health access may also deter businesses from locating in or expanding in a rural community, meaning fewer jobs that could lift rural residents up and make it easier for them to achieve good health. A 2006 Health Services Research article, The Effect of Rural Hospital Closures on Community Economic Health, reports that communities where the sole hospital closed saw both a reduction in per capita income and an increase in unemployment.
For a more in-depth discussion of healthcare access, see the Healthcare Access in Rural Communities topic guide.



