Rural Obesity and Weight Control
Obesity and overweight are ongoing health concerns nationwide. They are risk factors for a range of chronic diseases, including heart disease, stroke, some cancers, and type 2 diabetes.
Rural areas experience higher rates of obesity and overweight than the nation as a whole, yet many rural communities do not have the resources to address this critical health concern. Rural healthcare facilities are less likely to have nutritionists, dietitians, or weight management experts available. Rural areas may lack exercise facilities and infrastructure to encourage physical activity. Access to healthy and affordable food is also limited in many rural communities. Additionally, the distance that many rural residents must travel to access healthcare facilities, exercise facilities, and healthy food is an ongoing barrier.
To address these challenges, rural communities can invest in facilities and infrastructure that support access to healthy food, fitness, and healthy lifestyles. Communities may also choose to develop programs and services that help rural residents learn about the health risks of overweight and obesity, as well as adopt healthy lifestyle behaviors to control their weight.
Frequently Asked Questions
- How do rural areas compare to urban areas regarding obesity rates?
- Are rural children at greater risk of obesity and overweight?
- What are some factors contributing to rural obesity?
- How does obesity impact health?
- What can rural healthcare providers do to address obesity and overweight?
- How can local public health agencies help prevent obesity?
- What role can rural schools play in encouraging healthy weight?
- What can rural communities do to help reduce obesity?
- Where can I find examples of obesity prevention or weight control programs that work in rural areas?
How do rural areas compare to urban areas regarding obesity rates?
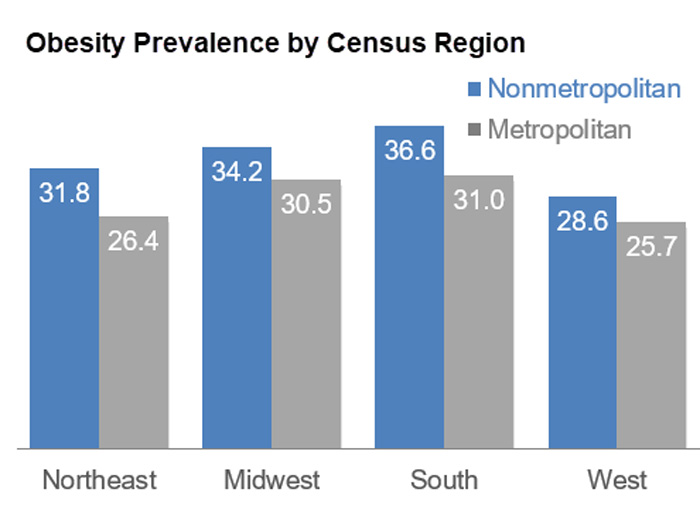
Obesity Prevalence Among Adults Living in Metropolitan and Nonmetropolitan Counties — United States, 2016 reports that, based on self-reported height and weight responses to the 2016 Behavioral Risk Factor Surveillance System (BRFSS) survey, obesity is more prevalent among adults residing in nonmetropolitan areas (34.2%) than among adults residing in metropolitan areas (28.7%). The largest nonmetropolitan and metropolitan differences in obesity prevalence occurred in the South (5.6%) and Northeast (5.4%) Census regions.
A 2018 JAMA article, Differences in Obesity Prevalence by Demographic Characteristics and Urbanization Level Among Adults in the United States, 2013-2016, examined rural obesity based on measured rather than self-reported height and weight. This study reported that the prevalence of obesity among nonmetropolitan adults was 43.1%, compared to 42.4% for adults from small metropolitan areas and 35.1% for adults from large metropolitan areas.
Are rural children at greater risk of obesity and overweight?
Differences in Obesity Prevalence by Demographics and Urbanization in US Children and Adolescents, 2013-2016 reports a higher prevalence of obesity among youth aged 2 to 19 years old in nonmetropolitan statistical areas (21.7%) compared to youth in large metro areas (17.1%) and medium or small metro areas (17.2%). This report also found that severe obesity was more prevalent among youth in nonmetro areas (9.4%) than among youth in large metro areas (5.1%) and medium or small MSAs (5.3%).
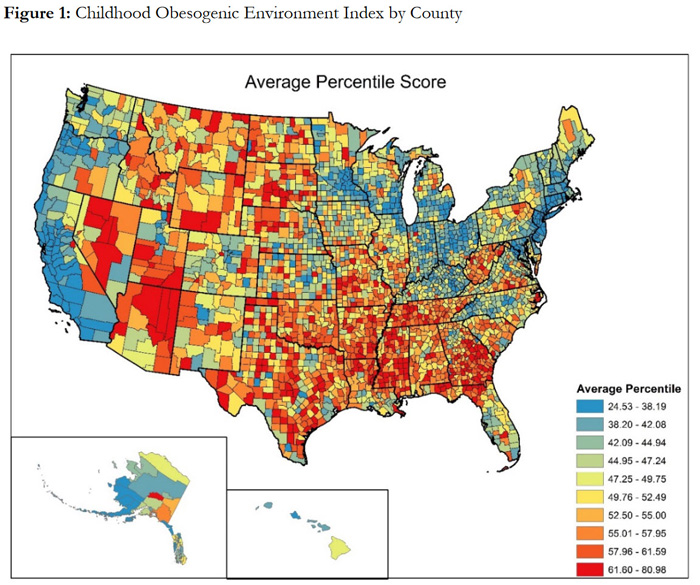
The context a child grows up in can influence the potential for a child becoming overweight or obese. A childhood obesogenic environment index (COEI), created by the University of South Carolina Rural Health Research Center, combines 10 factors related to obesity, including exercise opportunities and access to healthy foods, into an overall score. Based on this index, Development of a National Childhood Obesogenic Environment Index in the United States: Differences by Region and Rurality reports a higher average score for rural counties (52.9 points) compared to metropolitan counties (46.5 points), with greater values assigned to environments with an increased risk of childhood obesity. This map shows county-level data on average COEI scores in the United States.
What are some factors contributing to rural obesity?
Obesity and overweight have long been considered causes for concern in rural areas. The National Advisory Committee on Rural Health and Human Services (NACRHHS), in its 2005 Report to the Secretary, dedicated a chapter to obesity. In the 2011 NACRHHS Report to the Secretary, the committee focused on rural childhood obesity. The State of Obesity 2024: Better Policies for a Healthier America also reports that rural counties have a higher prevalence of obesity for adults and children than their counterparts in urban counties. Some contributors to rural obesity identified in these reports include:
- Influence of poverty
- Limited access to healthy and affordable food
- Higher calorie consumption
- Lack of nutrition education and services
- Limited access to obesity prevention programs and weight management services
- Fewer opportunities for children to be physically active in afterschool sports or events
- Scarcity of parks, recreational areas, sidewalks, bike trails, and exercise facilities that promote physical activity
- Reliance on automobiles to meet transportation needs, rather than walking or biking
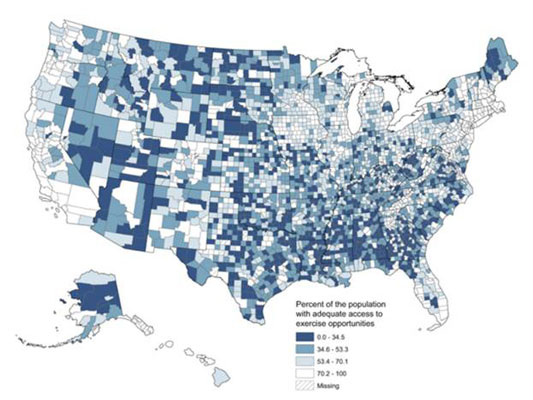
The USDA Food Environment Atlas shows metro and nonmetro data on issues such as food access, socioeconomic characteristics, food assistance programs, and built environment. The map below, from a 2015 Preventing Chronic Disease article, shows county-level access to parks and recreation facilities, based on data collected for the 2014 County Health Rankings and Roadmaps. Darker counties indicate areas where fewer residents have adequate access to exercise opportunities:
How does obesity impact health?
According to the National Institute of Diabetes and Digestive and Kidney Diseases, overweight and obesity increase the risk of several other health problems. These include:
- High blood pressure
- Type 2 diabetes
- Heart disease
- Stroke
- Liver disease
- Osteoarthritis
- Sleep apnea and respiratory problems
- Certain types of cancer
- Pregnancy complications
The higher prevalence of obesity and overweight among rural residents may be a contributing factor for higher rates of chronic diseases in rural communities. The Centers for Disease Control and Prevention's Health, United States, 2019 Table 13 reports higher rates of heart disease and cancer within non-metropolitan areas. The following rates are for 2017-2018:
| Metropolitan Area | Outside Metropolitan Area | |
|---|---|---|
| Heart disease | 10.4% | 12.5% |
| Cancer | 6.1% | 6.9% |
| Source: Health, United States, 2019. Table 13 | ||
For more information about chronic disease prevalence and treatment in rural areas, see the Chronic Disease in Rural America topic guide.
What can rural healthcare providers do to address obesity and overweight?
To address obesity and overweight, rural clinics and hospitals can offer wellness classes and activities that encourage healthy diet and exercise, such as sessions on nutrition, preventing heart disease, and controlling diabetes. Hospitals that have exercise equipment for rehabilitation may want to make their workout areas available to the entire community.
Primary care providers can serve as an information source to their patients on healthy diet and physical activity. The Agency for Healthcare Research and Quality offers a toolkit, Integrating Primary Care Practices and Community-based Resources to Manage Obesity: A Bridge-building Toolkit for Rural Primary Care Practices, to help rural primary care practices connect their patients to obesity management resources. In addition to offering a step-by-step process, the toolkit includes sample forms, worksheets, and other materials that can be adapted.
How can local public health agencies help prevent obesity?
Local public health agencies may find that by developing community partnerships with schools, healthcare providers, local businesses, and community groups, they can strengthen their mission to create opportunities for healthy living and reduce obesity and overweight in their communities. No one intervention or activity alone may solve the problem of obesity. However, when a variety of activities and programs are offered collaboratively, they can encourage and reinforce lifestyle changes that support healthy behaviors and reduce obesity. Projects or programs that can be conducted by public health agencies and their partners may include:
- Creating a community food policy council focused on healthy food choices as well as their availability and distribution
- Providing nutrition education and wellness classes for the community and schools to increase the consumption of fruits and vegetables and increase physical activity
- Working with local grocery stores and restaurants to help consumers make healthier choices by offering affordable and healthier foods
- Developing or expanding farm-to-institution programs in schools, hospitals, and workplaces
- Developing or expanding a farmers' market that is easily accessible within the community
- Partnering with schools to establish policies offering healthier food choices in the school cafeteria and in vending machines
- Promoting the maintenance of parks and recreational areas for walking, biking, and other physical activities for the entire community
- Collaborating with healthcare services, wellness centers, food vendors, and local businesses to support wellness events or health fairs
- Supporting community projects that make neighborhoods safer for outside activities including bicycle riding and walking to school
The Centers for Disease Control and Prevention's (CDC) Obesity Strategies: What Can Be Done identifies a variety of strategies to address obesity, including public health approaches for increasing physical activity, promoting healthy food consumption, and improving early care and education for children.
CDC also publishes Healthier Food Retail: An Action Guide for Public Health Practitioners. This publication discusses ways public health agencies can partner and coordinate with food retailers to support healthier eating and includes examples of obesity prevention initiatives that can be implemented at the local or regional level.
What role can rural schools play in encouraging healthy weight?
Schools can play a key role in encouraging healthy weight of children and adolescents by developing programs and policies supporting healthy lifestyle behaviors, such as good eating habits and regular physical activities. Schools can begin by offering healthy choices in school lunches, placing nutritious snacks in vending machines, and by providing learning opportunities that promote healthy eating and an understanding of good nutrition. Schools can also design physical education programs to encourage children to develop an active lifestyle.
From the Harvard T.H. Chan School of Public Health's The Nutrition Source, Healthy Schools discusses the role schools play in promoting healthy behaviors, and suggests policies and practices to encourage healthy eating and physical activity. Topics explored include:
- Increasing participation in school meals
- Promoting consumption of fresh fruits and vegetables
- Implementing nutritional standards for school meals and competitive foods
- Supplying adequate access to drinking water
- Providing sufficient active physical education
- Encouraging physical activity during recess
- Integrating physical activity with classroom instruction
- Developing comprehensive school activity programs
CDC's School-Based Obesity Prevention Strategies for State Policymakers identifies strategies, as well as policies, that have been shown to help address childhood obesity in schools. These policies and strategies include:
- Integrating school health services with nongovernmental entities
- Supporting the formation of health councils and use state and local data to guide decisions
- Supporting wellness policies and professional development opportunities for local leaders
- Investing in physical education and nutrition standards in schools
- Promoting student input and engagement regarding wellness policies
The most effective school programs are comprehensive ones that address food service, physical education, classroom education in the importance of healthy lifestyles and decision-making, and include community/parent involvement. The CATCH Program (Coordinated Approach to Child Health) is an example of a comprehensive obesity prevention program.
For additional information about the role rural schools can play in children's wellness, including nutrition and physical activity, see the Rural Schools and Health topic guide.
What can rural communities do to help reduce obesity?
Walking clubs, support groups for weight management, and healthy cooking and exercise classes are a few possibilities for supporting healthy weight throughout the community. Rural communities may want to develop a wellness center, bike trails, or walking paths to encourage healthy lifestyles, and/or work with neighboring communities to expand opportunities. Facilities may already exist in some communities that could serve the public as a community resource. For example, rural communities could enter into shared user-agreements with a local high school or community college opening their pool to the community for swimming, or gymnasium for early morning or after-hour community activities.
Several resources are available to help rural communities identify a suitable program to meet their needs:
- The CDC Guide to Strategies to Increase Physical Activity in the Community provides information for program managers and policymakers to help them select action plans that will increase physical activity within their communities.
- The Community Guide developed by CDC is a collection of evidence-based interventions in community settings to improve health and prevent disease. Searchable topics include obesity, nutrition, and physical activity.
- The Community Preventive Services Task Force's Built Environment Recommendation to Increase Physical Activity: Real-World Examples identifies examples of a combined approach of incorporating "activity-friendly routes" consisting of pedestrian, bicycle, and transportation systems with "everyday destinations" such as schools, parks, and city centers to increase physical activity within a community.
- Promoting Active Living in Rural Communities summarizes the characteristics of rural communities that may affect obesity and overweight, discusses observations from the field, and examines lessons learned from rural active living interventions.
Where can I find examples of obesity prevention or weight control programs that work in rural areas?
The Rural Health Models and Innovations section features examples of programs and interventions that have shown to be successful in preventing and reducing obesity and improving participation in healthier lifestyles. Examples include:
- Healthy Early Learning Project (HELP) – An integrated program addressing childhood obesity developed for public school preschool sites and Head Start sites in the rural Kansas counties of Marshall and Nemaha. Each site implemented a research and evidence-based program to increase physical activity and healthy food consumption of preschoolers ages 0 to 5.
- Win with Wellness – A partnership of county health departments, local healthcare providers, a regional nonprofit, and a medical school organized to develop weight-loss support groups and health education classes addressing obesity and chronic disease in rural Stephenson and Carroll counties of Illinois, where a large portion of the adult population in this rural area is overweight or obese, and the rates of diabetes, heart disease, and smoking are higher than in other parts of the state.

