Chronic Disease in Rural America
Chronic disease is a concern to rural healthcare systems and rural residents due to its impact on quality of life, mortality, and healthcare costs. The Centers for Disease Control and Prevention's (CDC) National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP) About Chronic Diseases webpage provides an overview of chronic disease in the U.S., detailing health and economic costs; prevention strategies; surveillance systems; and more. Rural communities have fewer resources to prevent and treat chronic diseases and conditions than urban communities, while facing higher rates of multiple chronic conditions, which are difficult and expensive to treat.
This guide will discuss the impact of chronic disease on rural America, how providers and communities can help patients with chronic diseases, and where to look for funding and opportunities to establish programs to address chronic conditions. Specific chronic diseases highlighted on this guide include:
- Heart disease and stroke
- Diabetes (Type 2)
- Chronic respiratory diseases
- HIV/AIDS
- Arthritis
For a more in-depth look at differences in health status for rural residents and contributing rural risk factors, see the Rural Health Disparities topic guide. See the Cancer Prevention and Treatment in Rural Areas topic guide for more on how cancer impacts rural residents and challenges related to prevention and providing cancer treatment.
Frequently Asked Questions
- How do rural areas compare to urban areas in terms of chronic disease prevalence and mortality?
- What contributes to higher rates of chronic diseases and conditions in rural areas?
- How can wellness and self-management programs help to prevent and address chronic diseases?
- What are strategies to ensure access to necessary care for rural residents with chronic disease? How can rural providers work with other healthcare facilities and healthcare professionals to address chronic diseases?
- How can rural communities and healthcare facilities work together to prevent chronic diseases?
- How can community health workers, home health providers, and school nurses help a patient manage chronic diseases?
- How can policymakers support rural communities' efforts in fighting chronic diseases?
- How prevalent are specific chronic diseases in rural America and what is being done to treat and prevent them?
- Are particular parts of the country more prone to certain chronic diseases?
- Where can I find grants to help start a chronic disease management program?
How do rural areas compare to urban areas in terms of chronic disease prevalence and mortality?
Rural areas face higher rates of chronic disease and related mortality rates. In some rural regions of the country and for some rural population groups, the disparity is particularly pronounced.
According to the National Center for Health Statistics report Health, United States, 2017 (Table 39), nonmetropolitan or rural residents report higher rates of multiple chronic conditions:
| Number of Conditions | Nonmetropolitan | Metropolitan |
|---|---|---|
| 2-3 chronic conditions | 22.6% | 18.9% |
| 4 or more chronic conditions | 5.1% | 4.2% |
| Source: Health, United States, 2017. Table 39 | ||
Rural areas tend to have higher rates for many of the most prevalent chronic diseases:
| Chronic Disease | Nonmetropolitan | Metropolitan |
|---|---|---|
| High cholesterol | 42.4% | 38.8% |
| High blood pressure | 38.1% | 32.6% |
| Arthritis | 31.1% | 25.1% |
| Depressive disorder | 20.1% | 17.5% |
| Asthma | 13.9% | 14.0% |
| Diabetes | 12.0% | 10.4% |
| Chronic Obstructive Pulmonary Disease (COPD) | 8.7% | 6.3% |
| Heart disease | 8.6% | 6.5% |
| Source: Chronic Disease Disparities by County Economic Status and Metropolitan Classification, Behavioral Risk Factor Surveillance System, 2013, Preventing Chronic Disease, September 2016 | ||
A 2017 Morbidity and Mortality Weekly Report (MMWR) article, Leading Causes of Death in Nonmetropolitan and Metropolitan Areas — United States, 1999–2014, reports that rural residents have higher age-adjusted death rates compared to their urban counterparts.
| Cause of Death | Nonmetropolitan | Metropolitan |
|---|---|---|
| Heart disease | 193.5 | 161.7 |
| Cancer | 176.2 | 158.3 |
| Chronic lower respiratory disease | 54.3 | 38.0 |
| Stroke | 41.5 | 35.4 |
| Source: Leading Causes of Death in Nonmetropolitan and Metropolitan Areas — United States, 1999–2014, Supplemental Tables, Morbidity and Mortality Weekly Report, 66(1), 1-8, January 2017 | ||
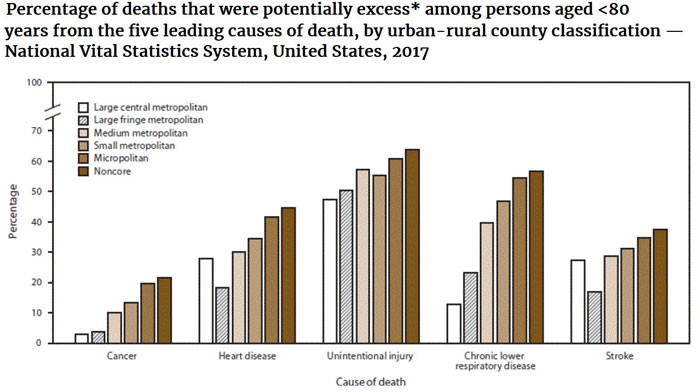
A 2019 MMWR article, Potentially Excess Deaths from the Five Leading Causes of Death in Metropolitan and Nonmetropolitan Counties — United States, 2010–2017, examines potentially excess deaths from cancer, heart disease, chronic lower respiratory disease, stroke, and unintentional injury, comparing data from 2010-2017 for 6 urban-rural county classifications. In this article, potentially excess deaths refer to deaths among persons under age 80 that exceed the expected death rate for each cause based on benchmark state-level data.
What contributes to higher rates of chronic diseases and conditions in rural areas?
Some contributing factors to the rural disparity in chronic disease include:
An Aging Population
As individuals age, their risk of having multiple chronic conditions increases and rural areas tend to have older adults as a larger percentage of the population. Table S0101 from the 2020-2024 American Community Survey 5-Year Estimates shows 22.0% of the noncore (small rural) area and 19.8% of the micropolitan (large rural) area population is 65 years of age or older, compared to 17.2% of the nation's population as a whole.
Health-Related Behaviors Related to Chronic Disease
A 2017 MMWR article, Health-Related Behaviors by Urban-Rural County Classification — United States, 2013, discusses how rural residents have a lower prevalence of several positive health-related behaviors that can contribute to chronic disease. Rural residents were less likely to be nonsmokers, maintain a normal body weight, and meet physical activity recommendations. The rates of these health-related behaviors decreased as rurality increased.
| Health-Related Behavior | Noncore | Micropolitan | Nation as a Whole |
|---|---|---|---|
| Nonsmoker | 74.9% | 76.5% | 81.0% |
| Normal body weight | 28.9% | 30.6% | 34.2% |
| Meets aerobic physical activity recommendations | 46.7% | 49.2% | 50.7% |
| Source: Health-Related Behaviors by Urban-Rural County Classification – United States, 2013, Morbidity and Mortality Weekly Report, 66(5), 1-8, February 2017 | |||
Environmental and Occupational Factors
Many industries in rural areas increase the potential for chronic disease, such as respiratory illness for miners, and prolonged exposure to chemicals and sun leading to cancer or other illnesses for agricultural workers. See What types of environmental hazards do rural communities face that endanger the health of their residents? on our Social Determinants of Health for Rural People topic guide for additional information on environmental hazards related to health.
Healthcare Access Barriers
Access to Quality Health Services in Rural Areas – Primary Care: A Literature Review, a section of the 2015 report Rural Healthy People 2020: A Companion Document to Healthy People 2020, Volume 1, discusses the connection between limited primary care access and poor health outcomes for chronic conditions such as cancer, diabetes, and heart disease. The literature review emphasizes that one of the important roles of primary care is screening for health conditions so appropriate treatment can be provided. For more information on barriers to accessing healthcare, see the Healthcare Access in Rural Communities topic guide.
Screening rates in rural areas often lag. Table 35 from the report, Health, United States, 2019, found that 61.3% of metro residents aged 50 to 75 years of age had a colonoscopy in 2018, compared to 58% of their nonmetro counterparts. To learn more about differences between rural and urban cancer screening rates, see How do rural areas differ from urban areas in their use of cancer screening? on our Cancer Prevention and Treatment in Rural Areas topic guide.
For more details on factors that add to cancer incidence rates in rural areas, see What contributes to higher incidence rates of cancer in rural areas and what can be done to reduce the risk? on our Cancer Prevention and Treatment in Rural Areas topic guide.
How can wellness and self-management programs help to prevent and address chronic diseases?
Wellness Programs
Wellness programs promote healthy habits through lifestyle changes, such as healthy eating and increased physical activity, and disease management practices. Schools, workplaces, healthcare facilities, and other community organizations can offer wellness programs.
Wellness programs may target a particular age group, population, or chronic disease. For example, Fit & Strong!® focuses on osteoarthritis in older adults. The StrongPeople™ Program serves older adults through community-based healthy living classes, including strength training, aerobic exercise, dietary education, and more.
Some wellness programs not only focus on the physical aspect of managing disease, but also the mental involvement. Trinity Hospital Twin City's Fit for Life program educates to counter obesity and diabetes through the body, mind, and soul. The curriculum was developed and is taught by one of hospital's family practice physicians, which lends more credibility to the program and interest from the community.
For additional program examples, see our Wellness, health promotion, and disease prevention rural health models and innovations.
Self-Management Programs
Self-management programs can help patients manage different aspects related to their chronic diseases. A 2012 Journal of Nursing Scholarship article, Processes of Self-Management in Chronic Illness, identifies the following self-management processes for patients with a chronic illness:
- Learning about their condition and related health needs
- Taking ownership of their needs by monitoring and managing symptoms, taking medications, keeping appointments, and other health-related activities
- Engaging in activities promoting health and minimizing the impact of the condition, such as eating healthy and being physically active
- Activating healthcare, psychological, spiritual, social, and community resources
- Adjusting to living with their illness
The Chronic Disease Self-Management Program (CDSMP), originally developed at Stanford University, is a widely used evidence-based approach that can be used by patients in rural and urban areas. The model consists of online and in-person workshops led by individuals who have at least one chronic disease. CDSMP includes action planning, problem-solving, decision-making, interactive learning, behavioral modeling, and social support strategies with the training and materials geared toward specific chronic diseases.
A 2014 Rural and Remote Health article, Qualitative Exploration of Rural Focus Group Members' Participation in the Chronic Disease Self-Management Program, USA, examined the experiences of rural participants in a CDSMP. Participants in the program reported prioritizing health behavior changes as a result of the program. Examples include increasing their physical activity and improving their eating habits. Participants found their CDSMP group to be a supportive environment for discussing their condition, an important factor in rural communities where those with a chronic condition may feel socially isolated. Peer Support for People with Chronic Conditions in Rural Areas: A Scoping Review, a 2016 Rural and Remote Health article, provides an overview of rural peer support programs that offer support to those with chronic conditions provided by someone with the same condition or otherwise in similar circumstances. These types of programs offer social support and skill development to participants, helping educate patients and increasing their chronic disease self-management abilities. The article offers recommendations for rural communities interested in developing a peer support program.
Unfortunately, many rural areas lack CDSMP programs. A report from the CDC, Diabetes Self-Management Education Programs in Nonmetropolitan Counties, 2016, found that 62% of rural counties did not have a diabetes education program. Similarly, Dissemination of Chronic Disease Self-Management Education (CDSME) Programs in the United States: Intervention Delivery by Rurality, a 2017 International Journal of Environmental Research and Public Health article, examined the availability and types of CDSME programs available in rural areas. The article identifies gaps in the CDSME program offerings and discusses challenges rural areas face delivering programming, including traveling long distances and related costs. For guidance on starting a rural self-management program, see the National Council on Aging's 2015 publication, Offering Chronic Disease Self-management Education in Rural Areas: Tips, Success Stories, Innovative Approaches, and Resources.
What are strategies to ensure access to necessary care for rural residents with chronic disease? How can rural providers work with other healthcare facilities and healthcare professionals to address chronic diseases?
There are many ways rural communities and healthcare facilities can support the health of individuals with chronic conditions:
Care Coordination
Care coordination models have been successful in improving rural patients’ healthcare outcomes through communication and planning involving healthcare providers, patients, and families. The Centers for Medicare and Medicaid Services (CMS) offers the Connected Care Toolkit to highlight the benefits of Chronic Care Management (CCM) and assist healthcare professionals in implementing CCM. Our Care Management Medicare Reimbursement Strategies for Rural Providers includes information for rural providers on billing for CCM services and other reimbursement strategies. For examples of care coordination programs, including the Patient-Centered Medical Home (PCMH) model, see Care Coordination Models for Chronic Disease Management within the Rural Chronic Disease Management Toolkit.
Integrated Service Delivery
Integrating behavioral health services with primary care can be an effective strategy to ensure rural residents with chronic depression or other chronic behavioral health conditions have better access to care. For example, Cross-Walk is a program in rural Michigan that provides access to counseling and treatment to address depression and substance abuse issues in a primary care setting. Our Rural Services Integration Toolkit provides information and resources to help rural communities and healthcare organizations integrate health and human services.
Transportation Services
Rural healthcare providers and communities can provide transportation to help patients with chronic conditions get to healthcare appointments and supportive services, such as wellness programs. Transportation options such as mobility vans, van pools, and local public transit can help patients access care within their rural community or reach specialty and subspecialty care available elsewhere. For more information on rural transportation and grant opportunities, see our Transportation to Support Rural Healthcare topic guide. For examples of transportation programs or guidance on program development and sustainability, see our Rural Transportation Toolkit.
Traveling Specialists
Programs that bring specialists and subspecialists to rural healthcare facilities can help patients with chronic conditions receive the care they require without leaving their community. A 2016 Journal of the American Heart Association article, Providing Cardiology Care in Rural Areas Through Visiting Consultant Clinics, highlights a program that increased access to cardiologists in rural Iowa through the use of a cardiology outreach program.
Telehealth
Telehealth can expand access to specialty and subspecialty care, as well as training for rural providers related to patients with chronic conditions. Project ECHO® — Extension for Community Healthcare Outcomes is a widely known and evidence-based program that connects primary care providers and academic specialists in a team to discuss care management and treatment for patients with chronic and complex conditions. Our Telehealth and Health Information Technology in Rural Healthcare topic guide has many resources on how telehealth can improve access to care in rural communities. For examples of telehealth programs or resources to help in developing a telehealth program, see our Rural Telehealth Toolkit.
Networking with Larger Systems
Rural facilities and providers may seek out relationships with larger healthcare systems or networks as a strategy to help their patients access needed care. This type of relationship, whether formal or informal, may facilitate and support access to traveling specialists, telehealth, and many of the other approaches listed above. Affiliation with larger hospital systems or networks is explained further in our Healthcare Access in Rural Communities topic guide question What are some strategies to improve access to care in rural communities?
How can rural communities and healthcare facilities work together to prevent chronic diseases?
Rural communities and healthcare facilities can work together to address common risk factors for many chronic conditions. Below are some approaches to help rural communities and healthcare organizations create an environment that supports healthy behaviors:
-
Support for Physical Activity
Walking trails, sidewalks, and parks are all aspects of the built environment that can encourage residents to be active. Rural communities can also develop programs to get residents moving such as the Albert Lea Blue Zones Project that created walking and biking initiatives in rural areas of Minnesota, or The Walking Classroom that incorporates walking with educational lessons multiple times throughout the week. -
Access to Healthy Foods
Community gardens, healthy cooking and nutrition classes, and exposure to healthy foods are all ways to support healthy eating practices among rural residents at risk for chronic disease. -
Tobacco Cessation
Encouraging rural residents to stop smoking and using other tobacco products is a valuable investment in preventing chronic conditions such as cancer and COPD. For more project examples, see our list of tobacco use rural health models and innovations.
Another aspect of prevention is early detection and treatment through health screenings. Early warning signs, such as high blood pressure or cholesterol, can help identify rural residents who would benefit from wellness programs or other interventions to prevent or control a chronic condition(s):
-
Screening Fairs
Communities and local healthcare providers can sponsor screening fairs to bring rural residents together for a common purpose of health and the prevention of chronic disease. Incorporating screening fairs into existing community events can be an effective way to reach rural residents who might otherwise not be screened. -
Mobile Screening Vans
Mobile healthcare vans are another method of providing health screenings to rural residents in communities where they live. Examples of mobile screening programs include The Health Wagon in rural Virginia and the New Mexico Mobile Screening Program for Miners.
How can community health workers, home health providers, and school nurses help a patient manage chronic diseases?
Community Health Workers
Chronic diseases require follow-up care, accountability, education, and preventive measures to better manage symptoms and disease. Community Health Workers (CHWs) fill gaps in the healthcare workforce to help provide healthcare services in rural areas. CHWs can play many roles in helping chronic disease patients in rural communities, such as:
- Providing wellness programming and education on chronic conditions and guidance on diet, physical activity, and smoking behaviors.
- Serving as patient navigators to help patients access their healthcare facility's services and to ensure the most appropriate care is provided.
- Offering counsel, support, and advocacy to patients and their families.
- Providing screenings and other basic services to patients.
The 2015 CDC policy brief, Addressing Chronic Disease Through Community Health Workers: A Policy and Systems-Level Approach, provides more information on the role of CHWs caring for patients with chronic diseases; policy options and steps states can implement to support the work of CHWs; and chronic disease program examples promoting CHWs as part of the public health workforce.
Our Community Health Workers Toolkit offers step-by-step guidance for rural communities interested in using CHWs to improve health in their community and includes information on model programs, training, sustainability planning, measuring CHW program impacts, and more. Additional information and resources on CHWs are available on our Community Health Workers in Rural Settings topic guide.
Community Health Representatives (CHRs) are trained, community-based healthcare workers who deliver health promotion and disease prevention services within their tribal communities.
Home Health
Home health providers offer a wide range of services for chronic disease patients in the comfort of their own homes. Many home health programs utilize remote patient monitoring (RPM) to manage patients with chronic diseases, many of whom might otherwise require a hospital stay. Home health services can also serve as an extra support to patients between clinic visits. RHIhub's Rural Home Health Services topic guide provides an overview of home health services in rural communities and discusses the availability of services and challenges they face providing home health care in rural areas.
School Nurses
School nurses help students with their overall health needs, including managing chronic conditions while in school. Nurses serve as a liaison between students, their parents, and healthcare providers. Since schools are a significant institution in the lives of children, partnerships between schools and local healthcare facilities provide an avenue to help children with chronic diseases manage their conditions on a regular basis. School nurses can also educate youth on healthy nutrition and physical activity habits, and chronic disease prevention. For more information on rural school nurses and student health education and prevention programs, see our Rural Schools and Health topic guide.
How can policymakers support rural communities' efforts in fighting chronic diseases?
Robert Wood Johnson Foundation's 2014 brief, Realizing Rural Care Coordination: Considerations and Action Steps for State Policy-Makers, outlines steps state policymakers can take to improve rural care coordination and features several state programs addressing rural chronic disease.
For an overview of policymaking to support rural health, see our Rural Health Policy topic guide.
How prevalent are specific chronic diseases in rural America and what is being done to treat and prevent them?
Heart Disease and Stroke
Heart disease and stroke are historically more prevalent in rural areas, and rural residents have higher death rates from these diseases.
| Rural | Urban | |
|---|---|---|
| Heart disease | 189.1 | 156.3 |
| Stroke | 39.0 | 36.6 |
| Source: Trends in Death Rates in Urban and Rural Areas: United States, 1999–2019. Data table for Figure 3. Age-adjusted death rates for the 10 leading causes of death, by urban-rural classification: United States, 2019. | ||
In 2017-2018, the prevalence of stroke in rural areas was reported as .1% lower than in urban areas for the first time, according to Table 13 of the National Center for Health Statistics report Health, United States, 2019.
| Nonmetropolitan | Metropolitan | |
|---|---|---|
| Hypertension | 38.1% | 32.6% |
| High cholesterol | 42.4% | 38.8% |
| Source: Chronic Disease Disparities by County Economic Status and Metropolitan Classification, Behavioral Risk Factor Surveillance System, 2013, Preventing Chronic Disease, September 2016 | ||
Prevention and Treatment of Heart Disease and Stroke in Rural Areas
A 2017 MMWR article, Reducing Potentially Excess Deaths from the Five Leading Causes of Death in the Rural United States, identifies rural tobacco use, lack of physical activity, poor nutrition, and obesity as contributors to high blood pressure and diabetes, which in turn contribute to heart disease and stroke deaths.
Rural community health programs focusing on nutrition, weight control, tobacco cessation, physical activity, and limiting alcohol use can help prevent heart disease and prevent stroke. Implementing strategies to target high blood pressure and high cholesterol, focusing on screening and intervention to help prevent or control heart disease.
Rural Heart Disease and Stroke Program Examples
- Health Coaches for Hypertension Control is an 8-week program providing hypertension management training led by community volunteers trained as health coaches to patients older than 60 years.
- Franklin Cardiovascular Health Program (FCHP) is a long-term study in rural Maine focused on heart disease prevention.
RHIhub Resources on Heart Disease and Stroke
Diabetes (Type 2)
Diabetes rates are higher in rural areas. The related risk factors for type 2 diabetes include obesity and physical inactivity, which tend to be more prevalent in rural areas.
| Nonmetropolitan | Metropolitan | |
|---|---|---|
| Diabetes | 12.0% | 10.4% |
| Source: Chronic Disease Disparities by County Economic Status and Metropolitan Classification, Behavioral Risk Factor Surveillance System, 2013, Preventing Chronic Disease, September 2016 | ||
For additional data on diabetes and prediabetes prevalence, see the National Diabetes Statistics Report from CDC's Division of Diabetes Translation.
Prevention and Treatment in Rural Areas
Rural programs supporting access to healthy foods and opportunities for physical activity aid in diabetes prevention efforts. Programs focusing on weight control and healthy living may also reduce obesity, a risk factor for diabetes.
Screening programs can help rural residents find out if they are at risk for diabetes, which can allow them to make lifestyle changes, increase their knowledge of diabetes, and receive medical care to help prevent the disease from developing. Screening programs can also help in targeting diabetes self-management education and support (DSMES) programs for rural residents with diabetes or at risk of developing the chronic disease. A 2017 MMWR Surveillance Summary, Diabetes Self-Management Education Programs in Nonmetropolitan Counties — United States, 2016, provides an overview of diabetes self-management education (DSME) programs in rural areas. The article reports, in 2016, 62% of nonmetro counties did not have a DSME program and the counties lacking a DSME program tended to be poorer and had higher rates of diabetes.
The CDC's National Diabetes Prevention Program works to prevent or delay type 2 diabetes in the U.S. and offers a lifestyle change program rural organizations can implement.
Telehealth can be used to help rural residents with diabetes access specialty and subspecialty care. Telehealth can also be a platform for patient education and chronic disease management skills.
Rural Program Examples
- Diabetes prevention programs, such as the Northeast Louisiana Regional Pre-Diabetes Prevention Program, work to reduce the prevalence of diabetes and/or slow the progress of the chronic disease in rural residents.
RHIhub Resources
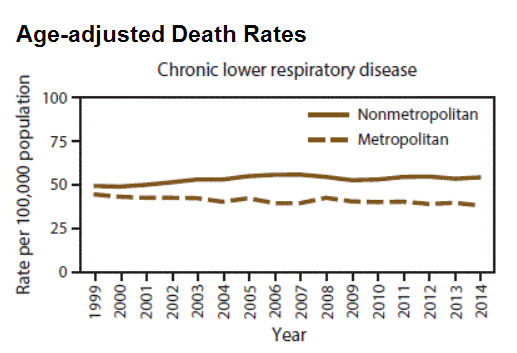
Chronic Respiratory Diseases
Chronic respiratory diseases, such as asthma and Chronic Obstructive Pulmonary Disease (COPD), make it difficult to breathe due to problems with the airways and other lung structures. Death rates for chronic lower respiratory disease are higher in rural areas, driven by a higher prevalence of COPD in rural areas. Despite having higher rates of COPD, rural communities are less likely to have pulmonary rehabilitation facilities. Similarly, rural communities also lack pulmonologists, who could provide guidance in the management of COPD, asthma, and other conditions.
| Noncore | Micropolitan | Small metro | Medium metro | Large fringe metro | Large metro center | |
|---|---|---|---|---|---|---|
| Adult prevalence | 8.2 | 7.6 | 7.0 | 6.4 | 5.3 | 4.7 |
| Deaths per 100,000 population | 54.5 | 52.8 | 47.0 | 41.9 | 36.2 | 32.0 |
| Source: Urban-Rural County and State Differences in Chronic Obstructive Pulmonary Disease – United States, 2015, Preventing Chronic Disease, February 2018 | ||||||
| Nonmetropolitan | Metropolitan | |
|---|---|---|
| Chronic lower respiratory disease | 54.3 | 38.0 |
| Source: Leading Causes of Death in Nonmetropolitan and Metropolitan Areas — United States, 1999–2014, Supplemental Tables, Morbidity and Mortality Weekly Report, 66(1), 1-8, January 2017 | ||
Prevention and Treatment in Rural Areas
The National Heart, Lung, and Blood Institute (NHLBI) identifies ways to prevent chronic respiratory disease by:
- Quitting smoking or not starting
- Avoiding lung irritants, such as dusts, chemical fumes, pollution, and secondhand smoke
Health-Related Behaviors by Urban-Rural County Classification — United States, 2013, a 2017 MMWR article, found that smoking increases with level of rurality. The report analysis found that only 74.9% of the noncore or small rural and 76.5% of micropolitan or large rural residents are nonsmokers, compared to 81% of the nation as a whole. Rural programs targeting tobacco use prevention and cessation are useful in addressing both direct exposure through smoking and exposure to tobacco smoke.
Environmental and occupational exposures are also risk factors for chronic respiratory diseases. Bringing Change for Rural COPD Patients: Possibilities with the COPD National Action Plan, a 2017 Rural Monitor article, provides an overview of COPD in rural areas and describes the types of exposures, in addition to tobacco smoke, that can result in COPD. Another 2017 Rural Monitor article, Pulmonary Health in Rural America: Cause and Impact of Work-Related Lung Diseases, offers an in-depth look at how occupational lung diseases, such as Black Lung or coal workers' pneumoconiosis (CWP), impact rural areas and discusses prevention strategies. A 2021 Rural Monitor article, Still Stealing Rural America's Breath: An Update on Chronic Obstructive Pulmonary Disease, offers an update on the National COPD Action Plan and highlights COPD rehabilitation and philanthropic efforts.
Rural patients with a chronic respiratory condition may find it more difficult to access the treatment, specialty, and subspecialty care needed to manage their condition. As with other chronic conditions, telehealth may help by providing access to subspecialists, and increasing rural providers' knowledge and education regarding chronic diseases. Learn more about COPD in rural areas:
Rural Program Examples
- New Mexico Mobile Screening Program for Miners offers health screenings to miners at risk for lung disease due to their profession and access to pulmonary subspecialists via telehealth if needed.
- See Rural Health Models and Innovations by Topic: Tobacco use for a variety of evidenced-based rural program examples addressing tobacco use.
HIV/AIDS
HIV prevalence is generally lower in rural areas than urban ones, but rural areas are also more likely to lack availability of HIV detection and treatment services. A 2021 Maine Rural Health Research Center chartbook, Rural HIV Prevalence and Service Availability in the United States: A Chartbook, provides data on disparities in access to HIV services between rural and urban areas, with rural counties less likely to have organizations providing prevention, testing, or treatment. A 2019 CDC National Center for HIV/AIDS, Viral Hepatitis, STD, and TB Prevention (NCHHSTP) slide set, HIV Surveillance in Urban and Nonurban Areas through 2018, provides detailed statistics on HIV and AIDS in rural areas. Regionally, the South is most impacted by diagnosed HIV infections for rural areas, followed by the Northeast.
HIV in the Southern United States, a 2019 NCHHSTP issue brief, points out that while the HIV epidemic in the South is primarily urban, 24% of new HIV diagnoses are in rural or suburban areas, which is a higher proportion than in other regions of the U.S. The brief also includes information and considerations on addressing HIV in rural communities.
| Population Size | Rate |
|---|---|
| Metropolitan Statistical Area (MSA), population over 500,000 | 433.5 |
| MSA of 50,000 – 499,999 | 206.4 |
| Nonmetropolitan | 143.3 |
| Source: HIV Surveillance in Urban and Nonurban Areas through 2018 | |
For additional county-level data on HIV and AIDS, as well as location information for testing and treatment centers, see AIDSVu.
Prevention and Treatment in Rural Areas
Just as in urban areas, rural HIV diagnoses are connected to sexual contact and injection drug use. Programs to prevent HIV infection may focus on abstinence, the use of condoms, safe sex, and the prevention of needle sharing, which can spread infections. Offering pre-exposure prophylaxis (PrEP) and post-exposure prophylaxis (PEP) medications can help prevent the spread of HIV. Those with an HIV infection can take antiretroviral therapy to help prevent passing the infection on to others. The AIDS Education and Training Center Program (AETC) National Coordinating Resource Center offers a Non-Occupational Post-Exposure Prophylaxis (nPEP) Toolkit with information on nPEP in rural America and perspectives from rural providers.
Screening for HIV infections is an important step in both prevention and treatment. Stigma and privacy are concerns are problematic in rural areas where there is less anonymity. Programs offering screening and treatment in a setting where other healthcare services are also provided can help patients more readily access treatment.
Rural patients diagnosed with an HIV infection may face challenges accessing specialty and subspecialty care. The use of telehealth is one promising method for both providing access to AIDS specialists and helping rural providers gain greater expertise related to HIV/AIDS. The National HIV Curriculum is a free educational resource for healthcare providers to help them learn more about HIV prevention, screening, diagnosis, and ongoing treatment. HIV Nexus is a one-stop location for information about HIV, including up-to-date tools and guidelines for providers, and educational materials for patients.
In recent years, clusters/outbreaks of HIV related to injection drug use have occurred in all regions of the U.S. in jurisdictions of varying urbanicity. Injection drug users are at a greater risk for infectious disease related to unsterile injections, including HIV, viral hepatitis, and endocarditis, an infection of the lining of the heart. Community responses to outbreaks often include infectious disease prevention supplies and services, including:
- Wound care supplies and sharps disposal kits
- Vaccinations
- Infectious disease testing, including home testing kits
- Referrals to infectious disease and substance use treatment and services
Adolescence is a critical period of time for the prevention of substance use that can progress into addiction. Adolescents with substance use disorders (SUDs) have increased rates of physical and mental illnesses, and poorer health and well-being overall. Teens can be at increased risk for HIV, sexually transmitted diseases (STDs), and teen pregnancy based on their experiences connected to four risk behaviors: sexual behavior, high-risk substance use, violence victimization, and mental health.
Ending the HIV Epidemic: A Plan for America provides an overview of the ten-year initiative starting in fiscal year 2020 to end the HIV epidemic in the U.S. and links to related federal resources. In addition, the HIV.gov resource What Is 'Ending the HIV Epidemic: A Plan for America'?, includes background information, goals, and discussion of the three different phases of the plan, with phase one focusing on 57 jurisdictions that include seven states with a substantial number of HIV diagnoses in rural areas.
Rural Program Examples
- Teens Linked to Care (TLC) began as a three-year pilot project in Indiana, Kentucky, and Ohio that sought to determine how prevention strategies and activities can be implemented to address substance use, HIV, and sexual risk behavior prevention among high-risk rural youth. The initial project was a collaboration between CDC's Division of Adolescent and School Health (DASH), the CDC Foundation, the Conrad N. Hilton Foundation, and three grantees. The second phase of the project started in the summer of 2019 with two grantees and will focus on behavior-based outcome evaluation and preventive health screenings.
- It's a Girl Thing: Making Proud Choices is a community-based education program focused on sexual health and STI prevention.
- The HIV Telehealth Collaborative Care (HIV TCC) Program, focused on rural veterans with HIV, uses telemedicine to help bridge the gap in HIV/AIDS healthcare services in rural communities.
- Project ECHO® – Extension for Community Healthcare Outcomes uses telehealth to connect rural providers with subspecialists.
- TelePrEP provides preventive care and PrEP medication through telehealth visits and prescription delivery services to prevent HIV infections in rural Iowa.
Arthritis
The 2017 MMWR article, Prevalence of Arthritis and Arthritis-Attributable Activity Limitation by Urban-Rural County Classification — United States, 2015, provides an in-depth look at the impact of arthritis in rural areas. Arthritis rates increase as rurality increases, with 31.8% of individuals in noncore rural areas, reporting physician-diagnosed arthritis compared to 20.5% of individuals living in large metro centers. One contributing factor to arthritis is age, but even age-adjusted rates show the burden of arthritis is greater in more rural areas:
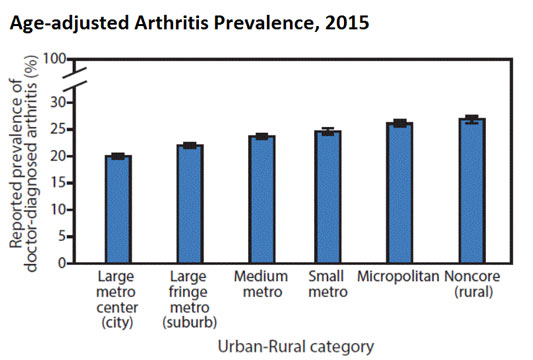
The groups most affected by arthritis in rural areas are the same as those most affected nationwide: older adults, women, people who smoke, people who are overweight, those who are physically inactive, and those with less education.
The same study reports that rural adults with arthritis reported higher rates of arthritis-attributable activity limitation, and this is true across different demographic and health behavior groups.
Prevention and Treatment in Rural Areas
The CDC identifies many risk factors for arthritis, including some that cannot be prevented or controlled, such as aging, sex, and genetics. Other risk factors include overweight and obesity, smoking, infections, and joint injuries. Given that obesity rates tend to be higher in rural areas, programs to help rural residents achieve and maintain a healthy weight are well-suited for preventing arthritis. Physical exercise is also helpful in addressing arthritis, though it can be more difficult in rural areas to find areas to walk or engage in a formal exercise program. The 2017 MMWR article mentioned above noted that self-management programs that are generally helpful for controlling symptoms, are less available in rural areas. However, self-directed versions of evidence-based interventions are available, and could be recommended by rural practitioners and supported by community service organizations. The same article discusses how rural communities and organizations can deliver effective self-management programs and support physical activity to help residents better manage arthritis.
Rural Program Examples
- Fit & Strong!® is an 8-week series of community-based physical activity and education classes to help promote and support patients with the self-management of arthritis symptoms.
- Chronic Disease Self-Management Program is a well-established program implemented in rural areas to address many conditions, including arthritis. The 6-week workshop provides skill learning and strategies for patients to better manage their chronic disease.
RHIhub Resources
Are particular parts of the country more prone to certain chronic diseases?
Certain regions and populations throughout the U.S. have particularly high rates of chronic disease. These health disparities (differences in health status compared to the population as a whole) are often associated with demographic and community-level risk factors such as limited access to healthcare facilities, low socioeconomic status, and low educational attainment. The following largely rural regions have well-documented health disparities for a range of chronic conditions.
Appalachia
Appalachia is the area following the Appalachian Mountains, stretching from Mississippi to New York. A 2017 Appalachian Regional Commission report, Health Disparities in Appalachia, examines mortality disparities related to chronic disease and risk factors contributing to chronic disease in the region. Mortality is higher in Appalachia for all chronic conditions included in the report and mortality rates in rural Appalachian counties are even higher:
| Nonmetro, not adjacent to a metro | Nonmetro, adjacent to small metro | Nonmetro, adjacent to large metro | Nation as a whole | |
|---|---|---|---|---|
| Heart disease | 234 | 219 | 218 | 175 |
| Cancer | 202 | 190 | 189 | 168 |
| Chronic Obstructive Pulmonary Disease (COPD) | 68.9 | 58.3 | 58.5 | 42.0 |
| Stroke | 46.0 | 45.9 | 44.6 | 38.4 |
| Diabetes | 27.7 | 26.4 | 24.7 | 21.5 |
| Source: Health Disparities in Appalachia, August 2017 | ||||
In terms of risk factors, rural Appalachian counties fare worse in terms of physical activity and smoking. Rural counties in the region also face more challenges for a range of social determinants of health, including poverty and education levels.
The Delta Region
The Delta Region includes 252 counties and parishes across eight states from Illinois to Louisiana. A 2015 Rural Health Reform Policy Research Center report, Exploring Rural and Urban Mortality Differences in the Delta Region, examines the leading causes of death for the region. The rural areas of the Delta Region fare worse for all the chronic conditions included in the report, compared to rural areas nationwide:
| Rural Delta Region | Rural, National | Nation as a Whole | |
|---|---|---|---|
| Heart disease | 248.4 | 195.0 | 171.3 |
| Cancer | 202.3 | 180.4 | 166.2 |
| Lower respiratory disease | 60.0 | 53.3 | 42.1 |
| Cerebrovascular diseases | 51.5 | 42.7 | 37.0 |
| Alzheimer's | 34.4 | 27.3 | 24.0 |
| Diabetes | 31.1 | 25.3 | 21.3 |
| Kidney disease | 24.1 | 15.7 | 13.3 |
| Source: Excel Workbook Tables: Mortality Rates among Persons by Cause of Death, Age, Region, and Rural-Urban Status: United States, 2011-2013, based on data from National Vital Statistics System (NVSS) via CDC WONDER. Part of the Exploring Rural and Urban Mortality Differences project, Rural Health Reform Policy Research Center. | |||
The Rural Delta Region Map Tool from the North Carolina Rural Health Research Program provides metro, nonmetro, and state-level data on obesity and diabetes prevalence, cardiovascular disease hospitalization, stroke hospitalization, and cancer incidence for the Delta region. To address the various social determinants of health (SDOH) that contribute to chronic disease in economically distressed counties of the Delta region, Delta Regional Authority works to improve quality of life through transportation infrastructure, basic public infrastructure, workforce training, and business development.
For more information on regional rural health disparities, or programs and statistics on rural health disparities, see our Rural Health Disparities topic guide. For more information on areas of the United States that are more likely to have cancer, see Are particular parts of the country more prone to cancer? on our Cancer Prevention and Treatment in Rural Areas topic guide.
Where can I find grants to help start a chronic disease management program?
RHIhub maintains a list of funding and opportunities related to chronic disease in rural America that is updated daily. The list includes past funding and opportunities that are currently inactive that may be available again in the future. You can also browse our Funding and Opportunities library and narrow by topic to identify opportunities related to chronic disease management or to specific chronic diseases, such as diabetes, chronic respiratory conditions, or cardiovascular disease.
If you need assistance finding funding and opportunities, contact the Resource and Referral Service at 800.270.1898 or info@ruralhealthinfo.org to request a free, customized funding search. You can also stay up-to-date on the latest funding and opportunity announcements by subscribing to the RHIhub This Week newsletter, RHIhub Daily & Weekly Custom Alerts, or to one of our funding and opportunities RSS feeds.
For more information about finding and developing grants in your rural area, see the Applying for Grants to Support Rural Health Projects topic guide.


