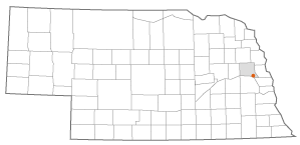
Historic Flood Cuts Off All Roadways to Rural Fremont, Nebraska: Hospital Plays a Vital Role in Coordinating Community Response
What Happened
On March 11, 2019, Winter Storm Ulmer, a record-breaking “bomb cyclone,” moved out of the Central Rockies, bringing hurricane-force winds with large amounts of snow and rain into the Great Plains. When the storm hit, above-average winter snowfall and below-average seasonal temperatures in the Midwest had already created conditions ripe for severe flooding. The result was flooding on a scale rarely experienced in the region, with some calling it a 100-year or even a 500-year event.
In total, at least 4 people lost their lives due to the storm and subsequent flooding, and it is estimated that over 1 million acres of farmland across 9 states were flooded. In Nebraska alone, the storm caused 2 deaths and over $3 billion in damage, affecting over 7,000 homes. Nearly every river in the eastern half of the state reached flood stage, with many reaching record flood levels, stressing dam and levee systems to the breaking point and causing multiple levee breaches and failures and one dam collapse. Roads, bridges, and highways, inundated by floodwaters, were closed, impassable, or washed away. Hundreds of thousands of residents were left without power for extended periods, often without ready access to food and necessary supplies.
A statewide emergency declaration was issued on March 11 in anticipation of the storm. Cities and counties stood up emergency operations centers and, in many cases, issued evacuation orders, including the northeastern city of Norfolk, which evacuated one-third of all its residents. As the flooding began, first responders worked around the clock, performing rescues and providing emergency care and aid for those trapped or stranded by floodwaters, as emergency shelters filled with residents leaving their homes to escape the flood. This unprecedented event presented emergency responders and response systems with substantial challenges.

The city of Fremont, with a population around 25,000, was one of the first places in eastern Nebraska to experience flooding from the storm. By March 15, flooding along the nearby Platte and Elkhorn rivers overran all major roadways into and out of Fremont, leaving the city in rural Dodge County a virtual island. For the next four days, the city was only accessible by air. Rich Oliva, Former Director of Security and a Certified Healthcare Emergency Professional (CHEP) for Methodist Fremont Health, reacted to the size and scale of the disaster by saying, “Who would've thought Survivor Island in Fremont, Nebraska!”
In the days prior to the city becoming isolated, the leadership at Methodist Fremont Health, which serves all of Dodge County and several neighboring rural counties, was carefully monitoring the situation and preparing for different contingencies. On March 11, the hospital stood up its incident command center, which was staffed solely by the emergency manager at that point. While flooding along the two rivers on either side of the city occurs in fairly regular cycles and is not uncommon, by March 14, the hospital had realized that this was not the usual cyclical event they had seen in past years. In response, they expanded the leadership team running the incident command center to include as many as 12-15 people, at times. Fortunately, unlike so many other buildings and homes in the city, the flooding never reached the hospital building, and patient evacuation was not required.
One of the first issues facing the hospital was staffing. As the floodwaters surrounded and cut off the city, many personnel stranded outside of Fremont were not able to get to the hospital to report for work. In some cases, hospital workers who left Fremont just for the afternoon on March 14 without knowing how quickly flooding would overtake the roads found themselves unable to return for several days. Therefore, ensuring that the hospital had adequate staffing became an early focus for leadership. In response, the hospital began to transfer some intensive care unit (ICU) patients — patients who would be treated at the hospital under normal circumstances — to partner hospitals in Omaha by ambulance. This “decompression” action enabled them to reduce staffing ratios down to one nurse to four patients or better and put the hospital in a better position to serve the community as events unfolded.
After moving these patients out of the hospital, the decision was made the next day, March 15, to move other patients in. The leadership team, based on an assessment of potential flood risk, decided to execute a horizontal evacuation of some residents from their long-term care facility, Dunklau Gardens, located on the north side of the hospital complex. In communications with the county road supervisor, they learned of an increased risk of a levee breach that would cause flooding along a small creek that runs just 50 feet north of the ground-level facility. If the levee breached and the creek flooded, the hospital would have at most two hours before floodwaters reached the building. Opting to take active steps to protect residents, rather than operating from a more reactive position, they issued the order to evacuate residents into the hospital's main tower.
To accomplish this, they followed the evacuation transport process the hospital already had in place. For each patient, the staff packed necessary items and compiled emergency transfer files, containing demographic information, plans of care, orders and medications, and other vital data. To avoid additional anxiety for patients during the move, leaders physically ran to different parts of the facility to verbally update and instruct staff, rather than issuing potentially stress-inducing mass alerts or alarms facility-wide. The residents were then moved to staging areas set up in Dunklau Gardens, where decisions were made about where the residents should be placed in the hospital. Once residents and staff reached their new locations, receiving groups were in place to help acclimate staff to a new working environment. They showed them where supplies and equipment were located and other key details that would make the transition smoother. In total, 8 residents were safely transferred. In the end, the levee, fortunately, did not breach and a full evacuation of the facility was not necessary.
Another key concern was the ability to access the supplies and resources necessary to continue hospital operations and make patient care possible. As standard practice, the hospital only keeps supplies onsite to maintain operations for a certain number of hours, generally enough for a few days. It became critical, therefore, to locate resources and determine how to get the supplies — typically transported by truck — to the hospital to replenish any that began to run low. In this case, Methodist Fremont Health was well-positioned; although not typical for a hospital its size, it maintains its own warehouse in the community. This facility, which is in a separate location from the hospital campus complex, contains certain supplies in large enough quantities to last multiple weeks.

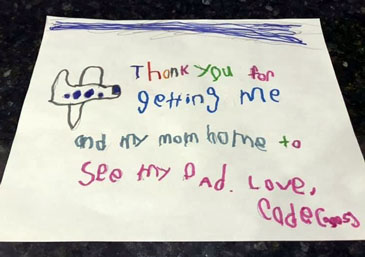
To transport other needed supplies, the hospital used relationships with local and regional partners. They coordinated flights with a large local helicopter company, LifeNet, which offered its services free of charge during the disaster. They also worked with one of their health system partners, Methodist Women's Hospital in Omaha, to have additional supplies flown in when needed. These flights also became a lifeline to maintaining and supporting a hospital staff working long hours under extraordinary circumstances. Additional staff members from Omaha were transported to Fremont to help relieve workers there, while those who had been on long shifts (and in some cases had even been sleeping at the hospital) were flown out to be reunited with their families and get some much-needed rest. This relationship was vital; as Oliva described it, “LifeNet became our taxi.” Without these services, it would have become more difficult to maintain the staff and resources necessary to keep the hospital running efficiently and responding effectively to the disaster.
While the leadership team's training and experience in emergency preparedness and response at Methodist Fremont Health was important in maintaining operations and levels of care at the hospital, that experience also enabled them to adapt their roles in different ways to meet challenges and fill gaps wherever needed in the community. This made them a valuable resource to the wider emergency response efforts happening in Fremont and the surrounding areas. Oliva, had over a decade of emergency management experience at the hospital and has worked as a firefighter and paramedic in Fremont, summed up the practical effect of this accumulated knowledge and relationships in this way:
“We saw how our experience in training paid off to assist our community, and when you've been around a while, you know who Joel and Lori and Brian and Shelly are…I've had the privilege for 20 years working with other leaders at other hospitals that when we got into these situations, it wasn't a matter of ‘What do I do here?’ It was just a matter of, ‘I need to call Bert, need to call Jason’…all these people, I just knew them by first name, and I knew what their resources were, and it made us that much more efficient at responding to it because of those relations.”
One area where this experience came into play was in the hospital's work with the emergency shelters. As the flood hit, local churches and schools began to turn their available spaces into shelters to take in those displaced by the flood. They soon realized, however, that providing care in the shelters would be an issue since many of the local public health department's staff had been stranded outside of the city. To address this situation, the hospital quickly put teams of nurses together to go out to the shelters to check on people's medical needs and provide care where needed. These “strike teams” identified sick or injured people and arranged transportation to the hospital for those in need of a higher level of care. They also provided vaccinations in response to possible tetanus infections and coordinated with doctors and pharmacists to replace prescriptions for people who no longer had access to their medications. This care was especially important in the first 3-4 days of the flood before any federal and national resources and aid could be mobilized and sent to Fremont.
Another way the hospital helped with community response was by sending out its language services team to work with the emergency shelters and first responders to serve non-English speakers. This was especially important when assisting with high-stress evacuation situations where clear communication between responders and evacuees was crucial to getting people to safety. Translators were able to give clear directions regarding evacuation procedures, such as safely entering and exiting rescue boats, and alerted responders to any needs and concerns of the evacuees, such as injuries or medical conditions they may have or the location of other people in need of aid.
In one illustrative case, the experience and connections of the hospital leadership contributed to a coordinated effort to locate and transport a bariatric chair to provide relief (and potentially avoid any further health complications) for an individual with a chronic health condition struggling to breathe in one of the local emergency shelters. The right equipment was identified at a facility in Lincoln, Nebraska, then brought in by a National Guard helicopter to Fremont and transported to the correct shelter by law enforcement. This effort involved around a dozen people, spanning multiple agencies and organizations, working together concertedly for close to 6 hours before finally delivering the chair. It was just one demonstration of how highly organized and coordinated efforts can succeed in providing for the needs of even a single individual in the midst of a large-scale disaster.

By March 17, road access to the west and south of Fremont had opened again on a limited basis. Hospital staff living south of the city, who had previously been unable to reach the hospital, were able to be shuttled to and from the campus using a military transport vehicle. This provided additional support for those who had been at the hospital working since the onset of the flood. Response efforts would continue in the following days as the flooding started to recede. On March 23, the hospital closed down their incident command center and began the transition to helping the community deal with the aftermath of the disaster.
Success Factors
Regular Intensive Training in Emergency Preparedness
The biggest factor that contributed to their successful response to the flood was the continual training in incident command and emergency response that the hospital has implemented for its staff. Beyond having good policies and procedures in place, it was critical to practice these procedures in order to be prepared for the challenges of a real-world emergency or disaster. By participating in live drills and exercises on a regular basis, the staff gain a better practical, hands-on understanding of what they need to do in a given situation, why it needs to be done, and why it needs to be done in a specific way.
Oliva compared this preparation to a sports team holding a scrimmage to prepare for a game: “The scrimmage, that's us doing our exercises. You can have all the playbooks in the world, you can read all the playbooks, but until you run a scrimmage, you're not going to understand how it works. And then the game is like the disaster because the disaster throws things at you that you weren't expecting, and which page of the playbook's going to come into play here?” The readiness achieved through this type of training enabled them to spend less time adapting or figuring out what they needed to do when the flooding occurred. Instead, they could focus on implementing the skills and know-how that they had already developed.
It is important to make sure all staff participate in the training exercises and that they learn both their specific role and how that role fits into the whole response effort. This approach to training helped make the staff more flexible and capable of filling different roles during the flood response.
As the flood demonstrated, in an emergency, many staff may not be available as they are also affected by the disaster, and other people must take on duties beyond their normal ones. Oliva gave the example of a situation in which staff may take on an unexpected role: “You may have a floor nurse that ends up running the operations section and overseeing all the nurses for a while. And she never thought she or he was going to be doing more than taking care of a few patients.” Building a broader understanding of preparedness and response through training helped give staff the knowledge, skills, and confidence to take on new roles in a real-life emergency.
Systems, Planning, Partnerships, and Collaboration
Another factor that contributed to successes in their flood response was the quality of the systems and planning in place prior to the disaster. One important aspect is Methodist Fremont Health's participation in the Omaha Metropolitan Healthcare Coalition (OMHCC). The coalition was established in the 1990s through the Metropolitan Medical Response System (MMRS) program. Oliva described it as “one of the few gold standards for MMRS in the nation.” The coalition has been hospital-led from its inception, and this has led to a strong healthcare focus in OMHCC's emergency preparedness and response activities throughout its existence.
In Oliva's view, Methodist Fremont Health has benefited greatly from the high level of integration that the hospitals in the coalition have. The relationships and interconnectedness developed through participation in the OMHCC meant that the hospital had the resources and support structure to step in and play a strong role in response and recovery efforts during the 2019 flood event. Oliva explained the significance of their involvement with the MMRS as follows: “Having myself and others do this and be involved with these exercises and development of plans for five county regions, nineteen hospitals, and not just checking the boxes, so by excellent involvement and the processes and procedure led to, I think, greater success and less challenges.”
In 2018, the hospital had just finalized an agreement to join the Methodist Health System. Although they were still in the process of transitioning into Methodist at the time of the flood in 2019, being a part of the new healthcare system made coordination with system partners in the area that much easier and enhanced the resources they could bring to bear on the situation. The collaboration with Methodist Women's Hospital — organizing flights to taxi staff to and from the hospital — is just one example of where this decision made a difference. Helping facilitate patient transfers, when needed, and ensuring that trucks with additional supplies from the system's shared services were available as soon as roads were open were among some of the other ways that this relationship provided valuable support.
At the local level, the relationships formed over the hospital's many years in the community were also vital to a successful response to the flooding. The hospital utilized these long-standing relationships to coordinate effectively with a wide range of agencies, groups, and organizations in Fremont, including the public health department, the airport, first responders, law enforcement, the public schools, local businesses, churches and faith-based groups, and even local airboat clubs. Without establishing these connections and building trust within the community, the hospital would have had limited ability to provide care and deliver services when needed most.
Leadership at the Ground Level
A final success factor was the decision-making and support provided by hospital executives both prior to and during the disaster, which was essential to enabling staff to perform effectively in an emergency response situation. The decision, first of all, to devote significant time and effort toward emergency preparedness, such as through participation in the OMHCC and engaging staff in meaningful, well-rounded training, laid the groundwork for success when put to the test in 2019. During the flood, the hospital CEO and administrative leaders took a ground-level approach to managing the situation. Oliva recalled, “Our executives spent just as much time on the floor or in the ER or, because we have a long-term care unit here, walking through those areas and talking to those people…They didn't sit in incident command. They didn't ask other people, ‘how are they doing out there?’ No, they were out there, you know, many, many times throughout a shift seeing for themselves, talking to people, and getting their own personal insights of how people are doing.”
This ground-level perspective was especially important in recognizing the stress that staff members were working under, as they did all they could for their patients and community, while often coping with the very same effects the disaster was having on their own homes and families. Understanding this pressure in such a close and personal way informed their decision-making as they worked to provide as much support and relief for the staff as possible. Whether it was making sure staff got breaks and rest when needed, helping staff to contact family members, or arranging flights for staff in and out of the hospital, they sought to actively care for their staff as they went about the difficult work of caring for the community.
Barriers
Maintaining Clear Communications
A significant challenge faced by the hospital in their response efforts was in the area of communications. As their flood response got underway, the hospital was communicating with the county emergency operations center (EOC) and other coalition partners through the existing OMHCC communication radio system. Issues arose when they discovered that communication over the system was not encrypted and therefore any transmissions could be picked up by people outside of the coalition. Members of the media and general public, who were anxious for information about the emergency response, began following these communications. It became easy for details that had been taken out of context, misinterpreted, or misunderstood to then be quickly amplified and spread over social media.
In one case, the decision to transfer some patients to Omaha was misconstrued into the idea that the hospital was being evacuated. This information was even found on an online posting board for a state agency. This misunderstanding was posted on the board for three days before it was taken down. Clear, reliable communication is essential in an emergency, and distortion of information can disrupt response efforts in multiple ways. To address this problem, the hospital and the coalition rapidly switched to a radio system that provided encryption and were able to reduce the instances of incorrect or incomplete information getting out into the public sphere.
Lessons Learned
Knowing Your Organization's Capacity
The 2019 flood presented the Fremont community and Methodist Fremont Health with a unique set of challenges. The experience of being cut off from outside support, essentially becoming an island in the middle of the country over several days, offered valuable lessons to strengthen their preparedness against any future emergencies. They realized the importance of understanding their organization's capacity to operate independently. After road access to Fremont was lost, the hospital had to rely on their own capabilities and local resources to respond to the situation in the time period before state and regional support could be organized and reach the city. National and federal resources would take additional time before they were available on the ground. Oliva pointed out that while The Joint Commission requires hospitals to list their capabilities of sustaining operations on their own for 96 hours, this does not mean that hospitals are required to have enough resources on hand to be fully functional for a 96-hour period. Rather, they must have a clear understanding of their own capacity and planning in place that will enable the hospital to meet this requirement in a situation where access to outside supplies and resources becomes limited.
For Oliva and hospital leadership, the flood brought a new understanding of what this requirement means. He reflected on some of the factors they had to consider:
“It never sunk home for myself as deep as it had after the flood because here we were in this situation. So, what do you have? What's your census, how much staff are you feeding on top of the visitors that are stuck here and the patients, and how long can you last with all this? What's your local resources and what is your sustainability? If you're cut off from leadership, staffing, as well as resource capability, what resources do you have in your own community that you didn't realize you did before to fill in these gaps?”
Developing a sharp awareness of their own capabilities and limitations can therefore significantly impact an organization's ability to provide an effective response for their patients and community when resources and support that could normally be relied upon are — even temporarily — out of reach.
Advice
An important piece of advice coming out of this generational storm and flood event is that paying attention even to the smallest details can have a large effect on an organization's ability to respond and provide care and comfort to those impacted. In the course of events like those of the 2019 flood, various small-scale problems, issues, and developments are continually arising and dealt with quickly in the moment.
One example of this occurred when staff from one department were called upon to work in another area of the hospital. In some instances, these staff members found themselves locked out of rooms, supply closets, cleaning closets, or other areas. Because they were now working in an entirely separate part of the building, their badges needed to be quickly reconfigured to grant them access to the places and the things necessary to do their jobs properly.
Another example occurred several years before the flood during testing of a newly installed backup power system for part of the hospital that is designated to serve as a family reunification area in the event of a disaster. During a test of the new system, they discovered that the electronic controls on the sinks and toilets in the restrooms in this area did not function on the backup power system. If they had not caught this glitch at that time and had used the area for family members during the flood in 2019, people could have been left without access to running water or working toilets.
Details such as these can often be overlooked in the planning process, yet the problems they cause can be significant. The time and resources that it takes to address such problems in the middle of a disaster can make the response less efficient and diminish ability to provide for people's needs. The more that these details can be accounted for and integrated into emergency planning processes and procedures, the more prepared organizations can be when a disaster occurs.
Person(s) Interviewed
Rich Oliva, Former Director of Security, Certified Healthcare Emergency Professional (CHEP)
Methodist Fremont Health
Opinions expressed are those of the interviewee(s) and do not necessarily reflect the views of the Rural Health Information Hub.
