AUGMENT Tele-ED/EMS: A Telehealth Program to Support Rural Emergency Rooms and Emergency Medical Services in Vermont
What Happened
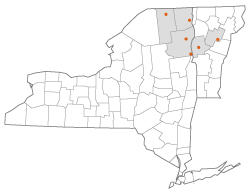
When Sarah Kessler, Miles Kittell, and Dr. David Nelson from University of Vermont Medical Center (UVM) envisioned a telehealth project that could supplement the peer-based assistance that rural hospitals and emergency medical services (EMS) agencies relied on each other for, they could never have imagined that it would be tested immediately or implemented in a virtual environment due to a global pandemic. According to Nelson, the UVM Health Network is a 6-hospital system in upper Vermont and New York state, which also includes home health and hospice, with the center of the network being located at UVM. The project, AUGMENT Tele-ED/EMS, was designed with UVM Medical Center at the center to facilitate tele-emergency management, tele-emergency medical services, and consults between emergency departments. AUGMENT Tele-ED/EMS stands for Advancing Unified Guidance for Medical Emergencies with Network Telehealth for the Emergency Departments and Emergency Medical Services of Greater Vermont. The project was born, according to Kittell, “when one of our emergency management physicians, Dr. Matt Siket, who is also a [board-certified stroke specialist] was staffing the telestroke service and found that a lot of times what folks needed, rather than a neurologist, was just a peer to parallel process things. So that idea led him to create AUGMENT and, with it, the idea of peer-based telemedicine emergency department support throughout the [University of Vermont Health Network].”
The project uses a hub-and-spoke model with the Vermont Medical Center as the hub and then all of University of Vermont Medical Center health network affiliate sites as the spokes. Kittel explained, “The project supports the mission of Vermont rural health organizations to expand access, coordination, and the quality of healthcare services using tele-emergency medicine (Tele-EM).” Kittell said the goal of the project was to support the other facilities and services: “We have resources, so why not utilize them, and especially with the pandemic and everything, telehealth is a huge resource.”
The goals of the AUGMENT Tele-ED/EMS project were to:
- Improve quality measure performance with stroke, severe heart attack (specifically, ST-elevation myocardial infarction, or STEMI), and trauma
- Increase rural site provider comfort with complex illness and pediatric emergencies
- Provide disaster surge support and parallel processing by enhancing staffing virtually
- Provide peer-based decision support to reduce the number of specialist consultations
- Increase emergency management services at rural sites, thereby reducing interfacility transfers and generating revenue for those sites while consolidating overall healthcare costs
- Reduce unnecessary ambulance transports through enhanced prehospital medical direction
- Improve rural emergency management provider wellness by reducing a sense of isolation and increasing support and network integration
The AUGMENT Tele-ED/EMS project is a 4-year, $1.2 million federally funded grant. The first part of the project involved a lot of credentialing and licensing of emergency physicians, which was made more cumbersome by the pandemic. Next, a telehealth hub, consisting of a computer, double monitor screens, a microphone, and a camera was set up at the UVM emergency department. Telehealth carts with high-quality cameras and equipment were deployed at each of the affiliate facilities, so a cart could be wheeled into a patient's room when needed.
Kittell outlined a theoretical situation where the telehealth network could be helpful and appropriate to use.
Kessler shared that while ED to ED was one part of the project, another fast-moving component of the project was ED to EMS. Using the same platform, EMS agencies in the field with a patient can connect with the ED. The project launched with a couple of standalone EMS squads and plans on adding 1-2 squads a month.
Success Factors
Nelson commented on one of the reasons the project was successful: “We're a very rural state with around 600,000 total residents and we have only one metropolitan area, which is around Burlington, and so we really are the quintessential rural state, but we're pretty homogenous in terms of working together in our emergency medical service (EMS) districts with even the hospitals not in our network — we receive patients from them.” However, Nelson pointed out that their health system is not the only health system in the state and that they work well with the other systems.
Another success factor Kittell pointed to was the paradigm shift that came with the COVID-19 public health emergency (PHE). For example, at the federal level, agencies like the Health Resources and Services Administration (HRSA) made funding available, and telehealth became much more accepted as a patient care delivery model. Kittell commented, “There was definitely more push from the top at UVM to bring on more telehealth initiatives.” He also spoke about the culture shift that has happened due to the PHE that has made it more common to jump on a video call or meet online.
Barriers
Virtual Implementation
Originally the project was going to include visits to remote sites, but the virtual implementation made this more difficult. Kessler explained that the grant originally included visits to each remote site to help them set up, but they were unable to do this due to COVID-19.
Broadband and Cellular Access
Another barrier the project team found was that providing hospital affiliates and EMS with the technology and the applications necessary for the AUGMENT project was not enough due to gaps in cellular service and Wi-Fi access in the state. Nelson added, “We could offer these services, all the technology the sites wanted, but if they can't connect with us, you know it's not very useful. So, we had to go back to the drawing board and say, ‘Okay, well, first, how do we improve your cell service and Wi-Fi services?’ We are a state with lots of hills and valleys and lots of dead zones.” Project personnel are working with state legislators to address the problem.
Lessons Learned
Early AUGMENT Tele-ED/EMS Outcomes and Successes
Some of the early outcomes, despite low volumes to date, according to Kessler, have been that patients have avoided costly and unnecessary transports and have received treatment closer to home and in their own communities. One of those cases involved a 3-year-old in respiratory distress. UVM performed a tele-ED visit with a smaller hospital and assisted the medical staff in stabilizing the toddler and avoiding a transfer to a larger healthcare facility. According to Nelson, the video consult helped the patient avoid a 2.5- to 3-hour drive. He added that this method could aid in the event of a disaster. “Whether it's 3 children or a busload of children, the medical system can't absorb everything. If you need air transport, you may be waiting for hours for transport.” He pointed out that smaller hospitals may have to manage patients for a time and allowing the larger medical center to assist and lay eyes on the patient can give them the confidence to do that.
Kessler added, “Just connecting the physician with the patient and the family and being able to make that decision together in the field, that's avoided some transports as well, making sure that everybody involved in that consult is comfortable with the decision.”
Making Affiliate Hospital Connections

One of the lessons learned related to working with the affiliate hospitals was the desire to connect with one another and not necessarily with the UVM. According to Nelson, “We set up this spoke-and-hub model for telehealth, where the affiliate hospitals would contact the university hospital for consults, but what we found is the affiliate hospitals wanted to talk amongst themselves and not always relate back to the university hospital. They wanted to interact with themselves so we're pivoting to what people want and trying to provide those services, rather than simply what we had initially set up.”
Emergency Telehealth Services for Children
One of the other outcomes of the AUGMENT project is that the team procured a grant from the Emergency Medical Services for Children Innovation & Improvement Center (EIIC) to help with implementing emergency telehealth services for children in Vermont. “We had a small sub-project of AUGMENT that was helping outfit some of our rescue crew with telehealth services, which dovetailed to the large AUGMENT project and helped EMS agencies to interact with the pediatric emergency services at the UVM,” explained Nelson.
Future Project Expansion
The work began with the 6 affiliate hospitals, but the ultimate plan is to extend it to the whole state, including Critical Access Hospitals (CAHs). Nelson pointed out, “That's where the Vermont Healthcare Emergency Preparedness Coalition (VHEPC) comes in. This organization is well connected with the whole state and the needs of all the rural hospitals. The ultimate plan is to get the bugs worked out and then extend this to the entire state, in the smaller rural hospitals.”
Nelson shared that one of VHEPC's missions is to improve preparedness in the state. To do this, monetary grants are given out yearly. When the AUGMENT program is ready to roll out to the state, the goal is for the VHEPC to be able to assist with spreading the word and with possible monetary support.
Another outcome of the project, according to Kessler, was the ability to manage intensive care unit (ICU) beds. She explained that ICU beds are a precious commodity. For example, a smaller affiliate hospital had a patient who needed a higher level of care, and that patient would have taken the last ICU bed at the larger healthcare facility. Through the telehealth consult, made possible by the AUGMENT project, the medical team determined that the patient could be moved to the medical floor, which preserved the ICU bed for another patient in need who filled the bed later that day.
Person(s) Interviewed
Sarah Kessler, Manager Digital Health Services
University of Vermont Medical Center
Miles Kittell, Project Manager, Research in Emergency Medicine
University of Vermont Medical Center
Dr. David Nelson, Pediatric Emergency Physician
University of Vermont Medical Center
Opinions expressed are those of the interviewee(s) and do not necessarily reflect the views of the Rural Health Information Hub.
